With the seven-day working strategy, Hertfordshire aimed to improve the flow from the acute into the community, ensuring discharges are not delayed over the weekend while service users wait for a package of care due to processes outside of the Monday to Friday norm. This example of a local initiative forms part of our managing transfers of care resource.
Hertfordshire is a county comprised of a mix of high-density urban populations and large rural areas. Three NHS clinical commissioning groups (CCGs) work directly within the county, including West Essex CCG due to an acute trust serving residents of both east Hertfordshire and west Essex. In addition to several NHS acute and community trusts, Hertfordshire has many independent health and social care services operating in the area.
This local environment means that partnership working between organisations is essential to delivering health and social care in Hertfordshire.
Before implementing a seven-day working transformation, weekend working in adult care services (ACS) hospital discharge teams was inconsistent, relying on volunteers and overtime payments to ensure weekend shifts were sufficiently covered. Last minute scheduling put extra pressure on the days leading up to the weekend, and the inconsistency of practitioners assigned to weekend shifts meant that service users were often not receiving continuity of care or progression towards discharge over the weekend
The plan
With the seven-day working strategy, Hertfordshire aimed to improve the flow from the acute into the community, ensuring discharges are not delayed over the weekend while service users wait for a package of care due to processes outside of the Monday to Friday norm. By improving this flow, service users will spend less time deconditioning in a hospital bed, get home as soon as they are ready, and ultimately reduce long-term dependency on care by having the right care wrapped around them at the right time thereby maximizing their independence.
The first step towards seven-day working was a stakeholder engagement process. Initially this brought together heads of services from ACS, the four main acute trusts and community hospital teams across Hertfordshire, and the Integrated Discharge Team leads. Five in-depth focus groups were facilitated with heads of service and members of staff to discuss the aims and possibilities of the strategy. A questionnaire went out to every member of ACS staff to gather valuable input and to ensure staff knew that their voices and operational expertise were valuable and included in the development process.
From this questionnaire, it was clear that staff wanted to be more involved in designing the strategy. Staff working groups were created to discuss the details of seven-day working and implementation, including possible rota patterns, rules for managing shift swaps, and the necessary induction that would be required for staff working across different sites.
Following the engagement period, it was decided to work on a ‘one in eight’ rotation – all staff working one weekend every eight weeks. No additional funding was used to cover weekends; staff instead have days off during the regular working week. Weekends are staffed at lower levels than the weekday, with community hospital staff included in the rotation to cover weekend shifts at the main acute sites.
Implementation
The engagement process was vital to the successful implementation of seven-day working. Some staff were initially resistant, particularly because there was no financial incentive to make the change. Through continuous engagement and adjusting implementation details to reflect staff feedback, we were able to secure buy-in from all staff. Engagement during implementation included regular discussions with managers, open email inbox to report issues, quarterly reviews in first year, and a full review of the rostering schedule after a year to confirm it was still the best option for staff.
Preparation for the weekend was re-designed and now includes a conference call on Thursdays, including active discussions with commissioners to understand what capacity is currently available and what additional capacity may be necessary to support weekend discharge and care.
A new process for working through a full seven-day week was also developed. In general, weekend working had been considered separately from the ‘normal’ caseload and review process during the week. With the implementation of seven-day working, team managers overhauled the weekend process and ensured that cases were tracked and progressed consistently. There was an emphasis put on the importance of working across a full seven days and planning for the natural peaks and troughs that arise.
It is important to note that this focus on consistency doesn’t mean that work is the same on the weekend as it is during the week. Lower capacity on the weekends across the rest of the system is currently reflected in fewer ACS staff members on weekends, which means work needs to be adapted. For example, not all weekend ward rounds can be attended by ACS staff; instead, a process was developed to ensure all patients who were not medically optimised in the week (but may be identified as fit for discharge on a weekend ward round) are reviewed in another way on the weekend so necessary progress can be made towards discharge.
Weekend working processes are continually reviewed by team managers to ensure that work on the weekend continues to result in progress towards discharge and improved flow in the week.
One key challenge to the implementation of seven-day working has been the necessary interactions with the external system. Not all health and social care partners have begun seven-day working; those who have often show lower levels of capacity on the weekend. As a result, a fully-staffed ACS team still cannot ensure consistent flow and support on the weekend because the support necessary from the acute, transport, care providers, etc. is not yet consistent. To tackle this challenge, ACS has leaned into its ‘Connected Lives’ model, which promotes independence, self-reliance and positive risk taking; working within this model, ACS staff are encouraged to find creative solutions. Work is also being done to create incentive schemes to help other partners buy into seven-day working for the future and promote the trusted assessment model so organisations can
Another key challenge is the need for an internal culture-shift in how work on the weekends is perceived. Staff were originally hesitant to adopt seven-day working, especially without any financial incentive as other partner organisations were receiving pay rises. As discussed above, staff engagement when shaping the format of seven-day working was a crucial piece of creating buy-in and ownership by all staff. Adjusting the work environment to highlight the benefits of weekend working has also been successful. One acute trust team takes team lunch breaks on the weekends, encouraging all staff to eat together and order in food on occasion. This practice takes advantage of the reduced need for continuous ‘clocked-in’ staff to incentivise weekend working and promote a positive culture.
Outcomes
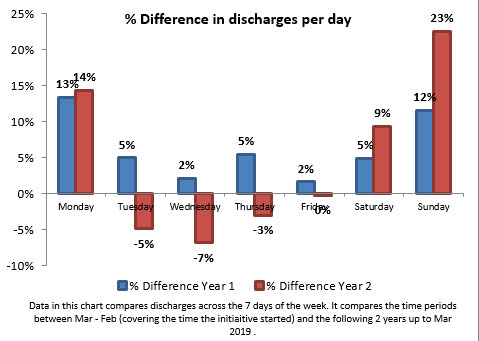
The quantitative results of seven-day working can be seen in the data following the first year after implementation in February 2017, as follows.
Number of assessment notifications have remained steady, but a noticeable difference can be seen in the number of discharges occurring not only on Saturday and Sunday, but also on Monday. This is evidence that the emphasis on seven-day working (rather than only separate weekend processes) has produced positive outcomes during the week.
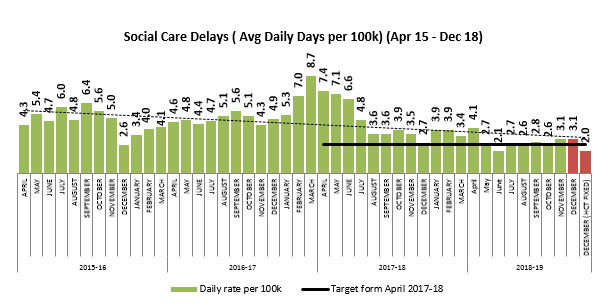
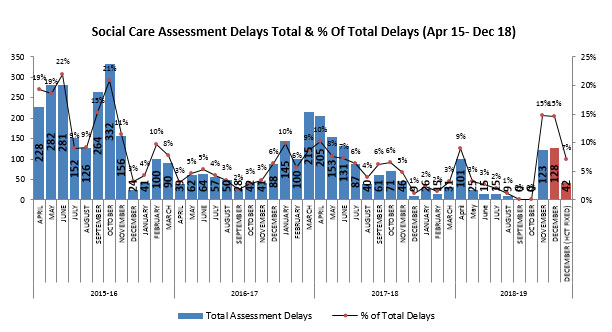
Social care delays have decreased over time after a spike in delays in winter of 2017. While this can likely be attributed to the combined impact of several different interventions that have been put in place over the past two years, seven-day working is certainly a driving force towards reducing social care delays.
Qualitative outcomes have also been seen. Though smaller teams on the weekend require regular processes to be adapted, team managers have reported that weekends provide them with an opportunity for more detailed oversight on the entire caseload. Being able to have time to stock-take on the weekend has shown benefits in monitoring caseloads throughout the week.
Consistency of scheduling throughout the full week has also allowed for effective overtime shifts on the weekend to respond to winter pressure. Before 7-day working was implemented, overtime was regularly used to cover weekends and it was difficult to find either the staff or the funding to increase staffing levels when necessary.
Next steps
It has been two years since seven-day working was implemented across ACS and one year since the last major review of its functioning. A new consultation is currently being planned to gather staff experiences and opinions to ensure the current scheduling rota and management process is fit for purpose. This will include tackling the issue of rotating staff and managers into sites and systems where they don’t normally work, which has made delivering a consistent process through the week difficult at times.
Work will continue with partner organisations to advance seven-day working across the system, especially those who are instrumental to the flow across the system on weekends.
Contact
Chris Badger
Deputy Director of Adult Care Services at Hertfordshire County Council, [email protected]