This case study forms part of the publication, Bespoke support for people with learning disabilities and autistic people, an evaluation on the impact consequence for local authorities and councils of delivering bespoke support to autistic people and people with a learning disability, including people who have been detained under the Mental Health Act (or at risk of being detained).
In hospital…they always locked the door. I wasn’t allowed to go anywhere. I wasn’t allowed in the kitchen. If I wanted to go somewhere the staff would say ‘I’ll call you when I’m ready’."
When my dad came to visit me, other people were jealous.
Now…My neighbours come and have a chat. When I moved in, they sent me cards. I work at a community fridge project, and I do it independently. I work in a charity shop for two days a week independently too. The staff are very pleased! I help to run an art and craft coffee group every week as well. I like to watch all the soaps on TV in the evenings. I can do most of the things in my home independently; cleaning and laundry. I just need help with using the cooker.
It’s important for staff to listen and be patient”.
Anna, Hertfordshire
Anna had spent five years out of area in a private secure hospital setting in Essex. During this time, she had very limited family and community contact. Previous community placements had failed, and she needed something much more bespoke. Anna’s home needed to be her own home as she struggled to share space and support with others.
The provider agreed to start working with Anna. They put together a bespoke support package proposal which included transition support from hospital to Anna’s new home. The proposal was initially rejected by the funders; however eventually it was agreed this was the best option for Anna. The provider worked with her in the hospital setting for a number of weeks until transition/discharge started. They sourced a rental property for her in the same town as her family.
The approach to developing Anna’s support was very relationship-based. The provider recruited a bespoke support team for Anna with similar interests to her. The provider changed things when certain aspects of support weren’t working for Anna. A good example of this was around the staff handover times and process. It was extremely triggering and challenging for Anna, so the provider developed ‘walk-by’ handovers, with all communication being done in written form between her support team, keeping the focus on Anna during the changeover of staff.
It was a huge adjustment for Anna. Although overall very positive for her, she was having to adjust to suddenly having many more choices and opportunities than she had been accustomed to in the hospital setting and she found this caused a high level of anxiety and also sadness after positive events such as holidays took place (and eventually came to an end).
Staff learned about Anna’s need for structure and routine to help her feel grounded and positive about her new life. They ensured they always had a clear plan with Anna following ‘big’ events, so that she felt she had new things to look forward to. This helped to minimise the experience of sadness at ‘good events’ coming to an end, which affected Anna quite deeply.
Anna had often experienced her personal belongings being taken from her room when she was in hospital. It took her a long time after moving into her own home to feel OK with putting her belongings out around her home. She would often hide things away in her room. Anna’s support staff were very sensitive towards this. They were patient and supportive until Anna trusted the safety of her new home and support arrangements, feeling ready to start putting her belongings out.
Anna’s risks began to reduce in comparison to the concerns around her safety at the time of her discharge from hospital. Robust risk assessments around the management of day-to-day items such as shampoo, prevented Anna from having free access to these items whilst in the hospital setting, but the provider observed many of these risks, and ‘behaviours of concern’ reduced significantly or disappeared completely once she was living in her own home with a bespoke approach to her support.
Perhaps the most significant change to Anna’s life was in her family relationships and involvement. For many years, Anna had a very difficult relationship with her brothers, and then her father died recently. Anna’s brothers were reluctant for her to attend the funeral. The support manager from Partners in Support initiated a sensitive conversation with Anna’s family, and she was enabled to attend the funeral. Not long after that, Anna had her 60th birthday. She held a big party to celebrate, and her brothers came; they were all amazed at the difference in her.
Anna has now been supported by the provider for 10 years. Anna is a big part of community life in her local area. She has a number of voluntary jobs, a good social life and a large network of friends. She has a stable support team, who are committed to working with her in a consistent and values-based way.
Anna has now been supported by Partners in Support to move properties a couple of times due to property issues, but the moves have all been successful, due to keeping the consistency of her support team around her.
The director of the organisation approached the local authority about 15 years ago. He wanted to do something different. He wanted to develop a support organisation which was smaller, localised and personalised to the people being supported.
Partners in Support was set up. It was a project approach which was developed jointly with the adult social care commissioning team initially, to help bring back people to area from long stay hospital settings. Everyone they support as an organisation have individual support packages. It is a completely bespoke approach.
As a provider, they have intentionally stayed small. There is now an E-brokerage service in place at the local authority using a provider framework which can make bespoke support approaches more challenging to deliver. This is because (as in the case of Anna) the provider was able to start from a blank page and use their experience and expertise with Anna to envision a support package that they thought would work best for her.
In the case of the E-brokerage service much of that work has already been undertaken and providers are usually being asked to bid for a finished plan, without necessarily having the option of engaging earlier in the process by working directly with individuals and families to develop bespoke support solutions.
People are still referred to the provider and individual contracts for support are set up on a ‘spot-purchase’ basis.
There is some flexibility within the spot contract arrangements in how they use people’s funding to provide flexible support. In some cases, they have been able to utilise funding to sub-contract to another activity provider in accordance with people’s goals and support preferences, so this is managed in a similar way to an ISF or flexible contracting arrangement.
For Partners in Support, it’s important that there are key leaders in local authorities with the appetite to make this happen, and willing to do things differently/outside of usual processes/payment arrangements.
As a provider, PIS have received ‘Outstanding’ in all KLOE areas of their CQC inspection, reflecting their outstanding commitment to outcomes and personalised support for the people they work alongside.
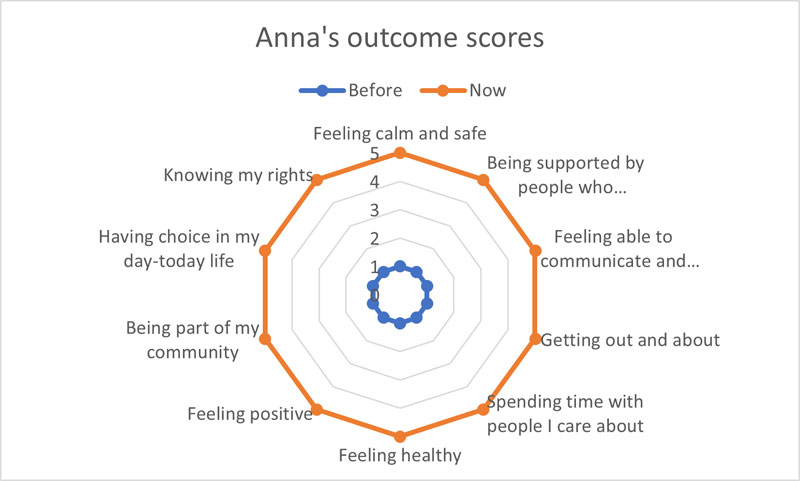
feeling calm and safe 1 before and 5 now.
being supported by people who understand me well 1 before and 5 now.
feeling able to communicate and being listened to 1 before and 5 now.
getting out and about 1 before and 5 now.
spending time with people I care about 1 before and 5 now.
feeling healthy 1 before and 5 now.
feeling positive 1 before and 5 now .
being part of my community 1 before and 5 now.
having choice in my day-to-day life 1 before and 5 now.
knowing my rights 1 before and 5 now.