This case study forms part of the publication, Bespoke support for people with learning disabilities and autistic people, an evaluation on the impact consequence for local authorities and councils of delivering bespoke support to autistic people and people with a learning disability, including people who have been detained under the Mental Health Act (or at risk of being detained).
I feel like I get really, really good support in my home. I’m really happy with the care provider, best in Essex!”
Rose, Essex
The provider received a referral for Rose because the hospital she was staying in was being closed suddenly.
There had been a news scandal about abuse of a patient with learning disabilities and autism in an inpatient setting, and the hospital provider had made the decision to close their inpatient unit suddenly. There had been an attempt to find another hospital bed for Rose.
Rose has a learning disability and is autistic. She had ended up in seclusion in a hospital setting which was unable to meet her needs, and where the nurses who were caring for her had no learning disability training. They did not understand how to support her.
The provider began attending the Care and Treatment Reviews (CTRs) for the patient, but no actions were ever implemented from the CTR action plan. In the provider’s experience CTRs don’t work because nobody is held to account. The plans are written after the meetings, but nobody is held accountable for the actions within the plan, and nothing gets progressed.
The provider has a direct contract with the NHS for Rose’s support. Rose’s property was purchased by an NHSE property grant; this is the same arrangement for the other people supported by the provider. The property is managed by a small housing association, which is locally based and selected by NHSE.
The provider completed their assessment of Rose’s needs, then the funding was agreed with a 50/50 split between social care and health.
There was a housing meeting, then an action meeting, led by health.
Health appointed a commissioner to deal specifically with Rose’s case.
A transition plan was agreed and implemented by the provider carrying out regular visits to spend time with Rose in hospital. Rose was on her own on a ward because she couldn’t be near other patients in the facility. Rose had been in seclusion for a long time and didn’t want to come out. The provider spent time with Rose, building trust and getting to know her slowly.
The provider doesn’t have difficulty recruiting staff because it has developed a good support model for the individual staff teams. Each individual support service has its own designated manager, who provides a robust support system for the staff team. There is a PBS (Positive Behaviour Support) trained lead in each support team, and a PBS practitioner who provides overarching support. This is built into the individual service design as part of the discharge planning process and is embedded within the service specification and contract.
Rose has her own team of dedicated staff and a manager who oversees her support team. The managers are now acting as PBS practical leads for the support service they oversee. There is a local team of PBS practitioners within the local authority area, who can provide overarching support.
The PBS practitioners are trained by the Tizard Centre. The provider believes that this level of training and insight for the staff teams supporting these individuals is preventing re-admissions to hospitals, because the individual support teams are trained and skilled to work with people who have complex behavioural support needs.
The provider shared that an important part of the success of the support arrangement is how the provider engages with parents and families. The families have engaged with their loved ones in the hospital setting in a very limited way for many years (perhaps visiting for an hour at a time in a visitor’s room) and don’t always understand what the person’s life is like day to day. There can be surprises when they are able to visit their family member at different times of day and are able to witness their different routines and how they react to their environment.
The families are often not prepared for what to expect in a supported living model, in terms of how the finances work, the costs involved with day-to-day living and maintaining a tenancy, and how decisions are made for their family member.
Family members themselves are often traumatised from the process of their relative being in hospital and there is often a lot of shame and guilt associated with the situation.
It’s important to recognise that although families want to be involved and help with decision-making, the voice of the person can sometimes be lost in the discussion. In these circumstances, independent advocacy for the person and family advocacy for the family may be helpful in representing the different perspectives.
The provider has noticed that there is a need to educate and train families on all these issues in preparation for the person being discharged from hospital.
The provider is a small, locally based organisation. It employs lots of staff to meet the high support needs of the people they support. Currently it supports both male and female clients with learning disabilities, who have been detained in assessment and treatment units and medium secure inpatient units. Most of these people had been in hospital between five to twenty years and had been victims of verbal and physical abuse whilst in hospital. All had experienced long periods of seclusion.
The provider doesn’t advertise their services. Referrals for the people they support come via word-of-mouth contact and positive working relationships with local commissioners. Referrals are often received via phone call from a commissioner, asking whether they can discuss the referral.
NHSE is the main funder for the people supported by the provider. The Dynamic Support Register identifies people who need support and are ready for discharge.
In the provider’s experience, different areas of the country are further ahead than others. The provider has worked in a number of cases where the people they support have been detained in hospital settings out of area. One commissioner called to discuss a referral with the provider and asked whether she could ‘come and look around’ at other people being supported by the provider, to gain an understanding of what support could be offered.
The provider explained that people are being supported in their own homes; and therefore, it wouldn’t be appropriate to show strangers around people’s own homes. They commented that there seems to be a lack of understanding about supported living for people with complex needs and risks at a decision-making level. In the provider’s experience, Essex is quite advanced in developing a joint commissioning approach. Essex had all of their ‘out of area’ people moved back into borough a number of years ago.
In Essex, they have an intensive support team for the families of people with learning disabilities and autism, and also the providers who are supporting people after discharge from hospitals. This helps to prevent crisis and/or re-admission to hospital.
In the provider’s experience, NHSE and CCGs are linking up better now. Five years earlier, it was completely different. Executives of NHS trusts seem to be more informed and getting more involved, and ministers are more involved than they used to be previously. The provider observed a commissioner putting out an alert recently to other commissioning bodies and chief executives around the country to ask for help and information. This is a positive development in joint working.
As a provider, My Life Choice have received Good in all KLOE areas of its CQC inspection.
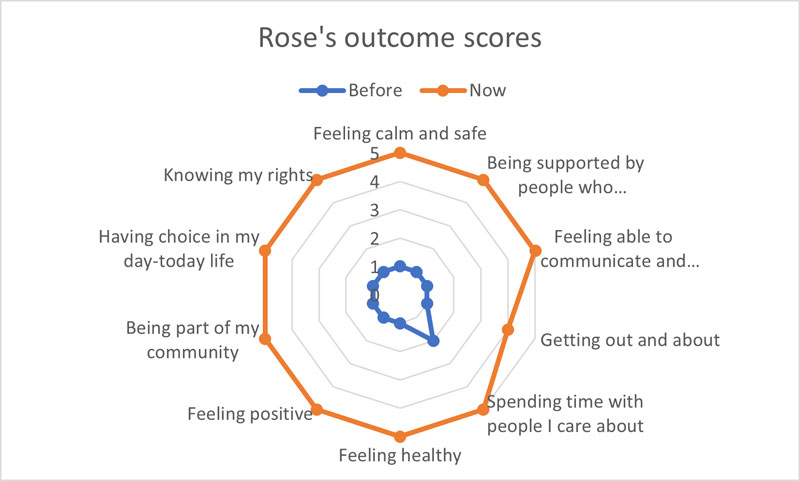
feeling calm and safe 1 before and 5 now.
being supported by people who understand me well 1 before and 5 now.
feeling able to communicate and being listened to 1 before and 5 now.
getting out and about 1 before and 4 now.
spending time with people I care about 2 before and 5 now.
feeling healthy 1 before and 5 now.
feeling positive 1 before and 5 now .
being part of my community 1 before and 5 now.
having choice in my day-to-day life 1 before and 5 now.
knowing my rights 1 before and 5 now.