Between October and November 2021, we undertook a national survey of Health and Wellbeing Boards (HWBs) with two core aims: to provide a snapshot of the extent to which there is alignment and collaboration between integrated care systems (ICSs) and HWBs to inform our policy messages; and to capture the ‘burning issues’ facing HWBs; to identify the key challenges and potential gaps in our existing support offers.
Introduction
Health and Wellbeing Boards (HWBS) are a statutory forum where political, clinical, professional and community leaders from across care and health in a place come together to agree a shared vision and shared strategy to improve the health and wellbeing of their local population and reduce health inequalities. Established in 2013, they are an important component of health and care planning, especially for integration and addressing health inequalities. They are a point of continuity in the continual changes to the health and care landscape. In part, this is because they have carved out a unique joint leadership role at place, as well as the recognition of the further opportunities they provide to shape and influence the wider system to drive long-lasting improvements to population health and wellbeing. It is also because HWBs are committees of local authorities, which are not subject to the extensive restructuring that has characterised the NHS over the past ten years.
The Health and Care Bill, subject to Parliamentary process, will establish integrated care systems (ICSs) as a key driver for joining up care and health services within the NHS and improving collaboration between the NHS and other key partners, in particular local authorities. From July 2022, integrated care boards (ICBs) will be statutory NHS bodies, and integrated care partnerships (ICPs) will be statutory committees of ICBs. There are currently 152 HWBs in England, one for each local authority with adult social care statutory duties. Some of the 42 ICSs are place-based, aligned to local authority (LAs) boundaries; some are much larger and include several LAs within their footprints; in others an LA sits across more than one ICS, cutting across existing boundaries of England.
The Local Government Association (LGA) is the national representative body for councils in England and Wales. We work with councils, national government and national bodies to support, promote and improve local government. The LGA has a well-established support offer to HWBs, which is kept under review to ensure it remains responsive to their needs and delivers sustained improvements.
Between October and November 2021, we undertook a national survey of HWBs with two core aims:
- To provide a snapshot of the extent to which there is alignment and collaboration between ICSs and HWBs to inform our policy messages
- To capture the ‘burning issues’ facing HWBs; to identify the key challenges and potential gaps in our existing support offers
There were 59 responses, across all regions, types of council and with a range of geographical complexities. HWBs and systems have different levels of maturity in their relationships with ICSs and the survey results reflect this diversity. Going forward, it is important that we recognise and are responsive to the levels of maturity of the relationship between ICSs and HWBs to inform our policy messages and shape our support offer to work with LAs and their NHS partners for all HWBs to move towards the level of the best performing.
The following provides a summary of the headline findings by theme.
Full analysis of the survey responses
Collaborative local leadership
Reponses indicate HWBs are clear on their role and responsibilities with regard to improving health and wellbeing outcomes, addressing health inequalities, and the importance of having the right leadership and the right membership. Most respondents (93 per cent) thought their HWB was building on what already works locally to a great or moderate extent.
There was a strong sense that delivering better outcomes for local people is dependent on collaborative, effective partnership working at ‘place’. Ninety per cent of respondents thought their HWB showed collaborative local leadership to a great or moderate extent, and 88 per cent reported this included working with a wider range or partners such as police, housing or the voluntary sector.
Bristol ‘One City’ Approach: Within Bristol there are three Integrated Care Partnerships (ICPs) or place partnerships. To strengthen relationships and collaborative working, the three ICPs have recently become members of Bristol’s HWB, which is also part of the One City approach. The One City approach brings together a huge range of public, private, voluntary and third sector partners within Bristol. They share an aim to make Bristol a fair, healthy and sustainable city through extensive collaboration across the city. The HWB is in the unique position to influence on the wider determinants of health, for example, access to employment and housing.
Key HWB achievements
Respondents were requested to give details of their key successes as open text answers. The most commonly mentioned successes are partnership working; addressing health inequalities and wider determinants of health; and the development and delivery of strategies, shown in the word cloud.
The word cloud above shows the frequency of themes that emerged in relation to the main areas respondents felt their HWB had been successful. The main themes were partnership working; addressing health inequalities; delivering strategies; and prevention programmes.
Developing strategies that reflect local need
The majority of respondents reported that their HWB strategy was promoting a person (80 per cent, and a preventative, assets-based population health approach (86 per cent). Almost 75 per cent of HWBs had either recently updated their joint strategic needs assessment (JSNA) and joint health and wellbeing strategy (JHWS) (25 per cent) or were planning to do so (almost 50 per cent). However, all boards should ensure their strategies are based on the most recent data available and reflect current local need to drive the strategic direction for ‘place’.
The LGA’s improvement offer has, and continues to support HWBs to review, refresh and refocus their priorities. With the encouragement for all Integrated Care Partnerships (ICPs) to produce an interim integrated care strategy by December 2022, it is crucial that HWBs are clear on their local priorities in order for these to be taken into account at system level. Almost three in five (59 per cent) respondents said that their HWB is effective in ensuring that the community is involved in shaping its vision and actions that underpin its work to a great or moderate extent. While there is room for improvement in ensuring that all HWBs actively engage their communities, this forms a strong basis for HWBs to work with ICSs to ensure that strategic priorities set out in the integrated care plans are based on messages from place-based community engagement.
Diabetes Truth Programme: The London Borough of Merton HWB ran a Diabetes Truth Programme which was shortlisted for a Local Government Chronicle award. This involved innovative engagement of each HWB member ‘buddying up’ with a resident who had diabetes or was caring for someone with diabetes and had a series of conversations to help understand their lived experience and help them shape action to tackle diabetes locally.
The Big Leeds Chat: The Big Leeds Chat is a regular event hosted by Healthwatch. Using a range of different forums or methods, it brings together the most senior decision makers in health and care, working together as one health and care team to hear what matters to the people of Leeds.
Relationships with the wider system
There is appetite and a commitment by HWBs to engage in the changing health and care landscape. Almost three quarters of respondents (72 per cent) reported that they have effective working relationships and high levels of trust with ICSs to a great or moderate extent. Seventy three per cent were actively having discussions to ensure greater alignment with the Integrated Care Partnership (ICP). This is a positive finding and one which HWBs and ICSs need to build on to ensure a strong and collaborative working relationship between place and system leaders.
Whilst HWBs continue to operate as effective local partnerships and over three quarters (79 per cent) of respondents thought their Board was achieving best value, more needs to be done to ensure ICSs actively engage with existing place-based arrangements; and to have due regard for HWBs, JSNAs and JHWS in the development of their own priorities and plans. For example, only 36 per cent of respondents felt involved in influencing and shaping ICS strategies and investment plans. This finding is somewhat at odds with the response regarding the extent to which HWBs and ICP priorities are aligned. It suggests that informal discussions and ‘in principle’ agreements between HWB and ICS leaders are extensive in many areas but these currently have not developed into formal alignment of plans and strategies for place and system.
In respect of HWB engagement, some key member individuals are engaged and feed back to the Board, but there is no formal work currently at the level of ICS/ICB communicating with HWB as a whole or inviting formal, whole-Board input."
Comment from one respondent
Other comments indicated a lack of formal engagement of elected members at every level from district to county council.
Some HWBs also reported that they were unclear how they would fit into the new arrangements and this lack of clarity on their future role is causing concern.
HWBs have a significant role to play in the creation of ICPs. Where an ICS covers more than one unitary footprint, HWBs are likely to have a greater influence on the priorities and plans of the ICS if they collaborate with neighbouring HWBs to identify shared priorities that are most effectively addressed at system level.
Only 38 per cent of respondents reported having effective partnership working arrangements with other HWBs within their ICS to a great or moderate extent, and some comments indicated it is not always clear how effective partnership working locally will be translated up to the system level. This collaborative way of working with other HWBs may be particularly challenging for HWBs with no history of joint working. But there are already well-established examples of HWBs working overcoming geographic, demographic and political differences to identify shared strategic objectives and priorities within an ICS footprint.
Kent County Council and Medway Council, with the NHS, have created a Joint Health and Wellbeing Board to cover the Kent and Medway Health and Care System to avoid duplication and to work collaboratively. All partnerships have agreed to subsume this Board into the new Partnership Committee.
Challenges of working with ICSs
The survey asked respondents to identify the three main challenges they faced in building effective working relationships with ICSs.
The open text answers provided by respondents were grouped into broad themes, the most commonly identified challenges were funding and resourcing issues; organisational and cultural differences; and ways of working together. The main themes are illustrated by the word cloud below:
The word cloud above shows the frequency of themes that emerged in relation to the three main challenges faced by respondents in building effective working relationships with their local health and care partners. The main themes are funding / resourcing issues; ways of working together; organisational /cultural differences; and unequal partnerships.
The pandemic has strengthened collaboration between partners, and respondents expressed a strong wish that these gains should be galvanized. However, the shared common purpose during the pandemic has been responding to immediate pressures. The challenge is how to maintain this shared purpose and commitment to joint working in the longer-term on preventative approaches to address inequalities and improve population health. There needs to be a shift in focus or, as one respondent commented, ‘we will continue to have a ‘sickness service’ not a ‘wellness service’’.
Differing governance arrangements between health and local government, and restrictive (and reduced) funding limit the ability of health partners to shift the balance of investment away from acute and inpatient care and support to preventative measures were cited as the two most common challenges facing HWBs working effectively with ICSs/health partners. ‘Currently only the NHS has clarity of its resources and ability to look into the near future to plan investment and service provision’.
Some comments in relation to accountability and decision-making indicated that processes to determine future governance arrangements are still in development. At the time of the survey, only two-fifths (42 per cent) of respondents thought their HWB is appropriately engaged in the local decision making in the ICS great or moderate extent. This is welcome but clearly needs to improve so that all HWBs are appropriately engaged in ICSs.
Recipe for success and key lessons
The survey asked respondents to share the key lessons learnt and their successes. The common themes are depicted in the word cloud below.
The word cloud above shows the frequency of themes that emerged in relation to the key lessons learnt from the challenges and successes they had identified. The main themes to emerge were build strong relationships; need for partnership working; need for community engagement; and need for clarity of role.
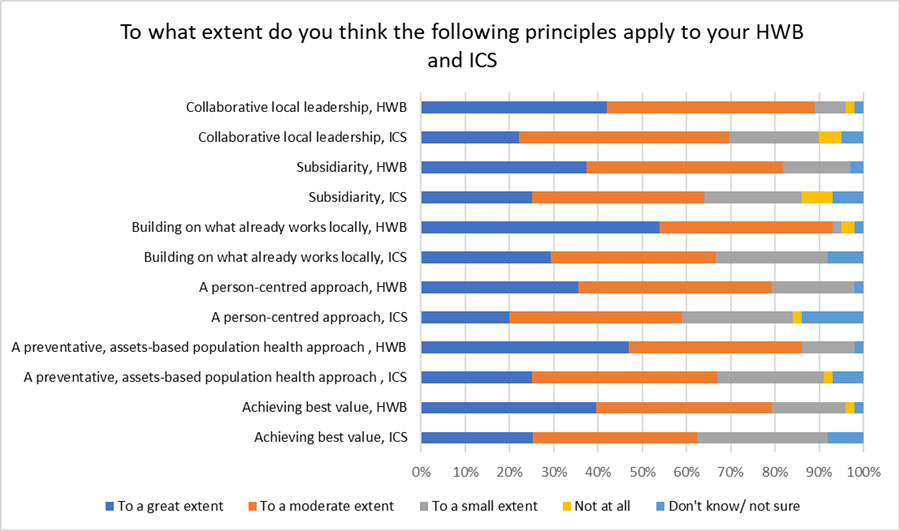
The essential ingredients in the world cloud strongly echo the emphasis on relationships, trust, and a culture of collaboration set out in the Integration White Paper. This approach is not new. In 2016 The LGA, NHS Confederation, NHS Providers, the Association of Directors of Adult Social Services and the Association of directors of Public Health agreed six principles underpinning effective integration. We asked HWBs to assess the extent to which they applied these principles and their view of the extent to which ICSs were underpinned by them. There was a marked difference in perceived application of them locally across the HWB and ICS. This finding strongly indicates that more needs to be done to ensure HWBs and ICSs develop a common set of principles to underpin the planning and delivery of integrated care.
To what extent do you think the following principles apply to your HWB
The chart above shows the extent to which respondents thought a list of principles applied to their HWB and ICS, their existing work and their existing work to establish integrated care. The data shown is outlined in the bulletpoints below.
- Nine in ten (90 per cent) of respondents thought their HWB showed collaborative local leadership to a great or moderate extent while 69 per cent thought so for their ICS.
- Four in five (81 per cent) thought their HWB was committed to subsidiarity to a great or moderate extent, and 64 per cent felt was the case for their ICS.
- Almost all respondents (93 per cent) thought their HWB was building on what already works locally to a great or moderate extent, as did 66 per cent in relation to their ICS.
- Four-fifths of respondents (80 per cent) believed their HWB used a person-centred approach to a great or moderate extent, with 59 per cent stating their ICS used this approach.
- 86 per cent felt their HWB used a preventative, assets-based population health approach to a great or moderate extent and just over two-thirds (68 per cent) thought this was used by their ICS. More than three-quarters (79 per cent) indicated that their HWB was achieving best value to a great or moderate extent while 63 per cent felt their ICS was achieving it to these extents.
What our support offer can help HWBs to achieve
The LGA has a long-established, well-respected Sector-Led Improvement approach to supporting and sustaining changes in local government. Adoption of this model as a means to effectively deliver system transformation and strengthen system leadership has gained traction in recent years; and there is growing recognition of the benefits it could yield within the NHS. Nationally, there has been a clear commitment from Government and NHS England and Improvement (NHSEI) to develop a support learning culture to develop appropriate leadership skills in ICS and place-based partnerships. The Care and Health Improvement Programme is funded by DHSC and NHSEI to provide a variety of bespoke support to health and care systems, including our specific offer to Health and Wellbeing Boards to:
- Develop and strengthen the role of place leaders giving them the skills and tools to be assertive and collaborative, both locally and with wider system partners, including neighbouring Health and Wellbeing Boards (HWBs) and the Integrated Care System (ICS), specifically alignment to the Integrated Care Partnership (ICP).
- Progress effective and sustainable partnership working through developing shared purpose, priorities, capabilities, governance and delivery arrangements in line with legislative proposals.
- Establishment of a HWB that drives the strategic vision for places, focused on addressing the wider determinants of health, creating the opportunities for health improvement, tackling health inequalities and promoting prevention.
- Successfully navigate legislative, performance and regulatory changes and challenges, as well as embedding gains made during COVID-19.
- Identify the points of influence within the wider system architecture to support the establishment of coherent, cohesive, and effective system-level partnerships that bring together ‘places’. For more information on how to access support, please contact us at [email protected].