This case study describes Rotherham’s progress developing integrated care arrangements. It is part of an evidence review commissioned from the Institute of Public Care.
Early leadership by the Health and Wellbeing Board, a clear and widely adopted Place Plan and a Place Board characterised by mutual trust and close working relationships are key factors in Rotherham’s transformation to an innovative and inspiring exemplar of best practice in integrating health and care.
A whole system shake up following systemic failure in relation to child sexual exploitation and the Alexis Jay and Louise Casey independent reports published in 2014/2015, prompted a new commitment to tackle poor population health and social and economic deprivation, led by the Health and Wellbeing Board. Integrating health and social care is one of their five priorities, managed through an Integrated Care Partnership. A comprehensive Place Plan clearly describes gaps, challenges, priorities and benefits and is easily understood by staff and public. Prevention, self-management, education and early intervention are top priorities - the ‘golden threads’ that run through the Plan.
Rotherham has given high priority to mental health and wellbeing. Recognising that mental and physical health are closely connected, joint care planning and support has been put in place and a successful programme of social prescribing makes good use of the local, well-developed and vibrant voluntary, community and social enterprise sector.
Strong partnership working between organisations is now in place, exemplified by positive leadership behaviours. Good links with the local university results in well evaluated pilots and new initiatives, providing a clear evidence base for change.
Introduction
It is useful to start the journey with a snapshot of Rotherham, taken from their Joint Strategic Needs Assessment
- Population 260,800 (2015) and forecasted to grow to 269,100 by 2025 (3.5%)
- Growth in the number of older people
- Increase in the number of people with long term conditions such as heart disease, diabetes, dementia and cancer
- Life expectancy below the national average
- Rotherham people live longer with ill-health and/or disability than England average
- Rotherham is becoming more ethnically diverse
- Significantly higher than average deprivation, unemployment and long term unemployment.
The health of the Rotherham population is generally poorer than the English average. With a history of limited partnership working and the need to change highlighted by the systemic failure in relation to child sexual exploitation that came to light in 2014, a concerted effort was made to forge bonds at the highest level and invest in developing a high functioning Health and Wellbeing Board. This included facilitated workshops to help partners understand each other’s issues and challenges and recognise and commit to the joint effort needed to address the health and care challenges in their local population. The Board has eighteen members from across the system including voluntary and community sector, Healthwatch, Police and Fire and Rescue and links across to the Rotherham Together Partnership and Plan with its five areas of interest:
- Building stronger communities
- Skills and employment
- Integrated health and social care
- Town centre
- A place to be proud of
The Joint Health and Wellbeing Strategy A Healthier Rotherham by 2025 describes the high level vision and four strategic aims to improve health and wellbeing outcomes in Rotherham that all partners have signed up to:
- all children get the best start in life and go on to achieve their potential
- all Rotherham people enjoy the best possible mental health and wellbeing and have a good quality of life
- all Rotherham people live well for longer
- all Rotherham people live in healthy, safe and resilient communities
The level of commitment of the partners is now described as being such that they put the collective aims of the Board above those of their own organisations. The Board both models and drives a whole system partnership approach from the top.
Governance, leadership and commitment
Rotherham’s health and social care community has been working in a collaborative way for a number of years. A key milestone in developing an integrated vision and plan for health and social care was the publication of the Integrated Health and Social Care Place Plan in November 2016. The Place Plan is now being refreshed and closely aligned to the aims in the Joint Health and Wellbeing Strategy: with the strategy setting the vision and direction for all health and wellbeing partners, and the Place Plan being the delivery mechanism for the ‘integrated health and social care’ elements. The common vision is articulated as:
“Supporting people and families to live independently in the community, with prevention and self-management at the heart of delivery”
The Place Plan does not replace partners’ individual plans but rather builds upon them by taking a common lens and identifying key areas for collaboration. The Plan links across to the South Yorkshire and Bassetlaw Integrated Care System (formally the Sustainability and Transformation Partnership) and is seen to be the best vehicle for driving though 80% of health and social care improvements in the Rotherham area (the remaining 20 per cent that concern specialist services is managed regionally). The Place Plan has also been turned into a lively animation that gets the key messages across in a fun and accessible way and has been an important tool in communicating with health and care staff and the public.
In 2017 a new high level partnership body was established reporting into the Health and Wellbeing Board: the Rotherham Integrated Health and Social Care Place Board now re-named as the Integrated Care Partnership Place Board. The Partnership is responsible for the delivery of the Place Plan and is co-chaired by the Chief Executive of the Council and Chief Officer of the CCG with membership of senior leaders from Adult Social Care, Public Health, the Hospital and Community Trust, Mental Health Trust, GP Federation, the umbrella organisation for the voluntary and community sector and the chair and vice chair of the Health and Wellbeing Board.
Development work was essential in enabling partners to get to know each other and formulate a common set of principles to encapsulate the agreed way of working going forward:
- Focus on people and places rather than organisations, pulling pathways together and integrating them around people’s homes and localities; we will adopt a way of working which promotes continuous engagement with and involvement of local people to inform this.
- Actively encourage prevention, self-management and early intervention to promote independence and support recovery and be fair to ensure that all the people of Rotherham can have timely access to the support they require to retain independence.
- Design pathways together and collaborate, agreeing how we do pathways collectively, to make our current and future services work better.
- Be innovative, using international evidence and proven best practice to shape our pathways to achieve the best outcomes for people in the most cost effective way.
- Strive for the best quality services based on the outcomes we want within the resource available.
- Be financially sustainable and this must be secured through our plans and pathway reform.
- Align relevant health and social care budgets together so we can buy health, care and support services once for a place in a joined up way.
Partnership members have spent time developing a culture of close working and peer support. Relationships are built on trust that has been established through understanding each other’s issues and ways of working, gained by spending time in partner organisations, seeing the world through a different lens and ‘walking in each other’s shoes.’ The result is a set of shared values including seeing the whole person and acknowledging the breadth of their needs - medical and non-medical and taking a whole system approach to change. The closely knit Chief Executive and Director-level leadership team meet weekly to problem solve together in the style of a high level action learning set and value the different perspectives that make them stronger as a team.
This group of leaders described “a melting pot of opportunity” which they are embracing with energy and enthusiasm, and it is this strong leadership that is now driving real change for Rotherham.
All health and wellbeing partners are also called to account on the Joint Health and Wellbeing Strategy and Place Plan by the Health Select Commission (health scrutiny), which adds another element of strategic overview.
Recent examples of successful joint working driven through this partnership are a reduction in delayed transfers of care from 6% to less than 2% and an 2017/18 winter plan to which all partners contributed resources on the understanding that A&E performance is about the whole system not just the hospital. The joint effort resulted in Rotherham being able to manage its winter pressures and was recognised as a national example of best practice.
Delivering integrated care
Rotherham’s Place Plan outlines five priority areas which the partners are working on collectively to transform the health and care system and improve the lives of local people. These 5 priorities are being delivered via 3 transformation workstreams:
- Children and young people
- Learning disability and mental health
- Urgent and community
These three workstreams are closely aligned to 3 of the aims in the Joint Health and Wellbeing Strategy:
- All children get the best start in life and go on to achieve their potential
- All Rotherham people enjoy the best possible mental health and wellbeing and have a good quality of life
- All Rotherham people live well for longer
Prevention, self-management, education and early intervention
Rotherham benefits from having a strong and vibrant voluntary and community sector of approximately 1,382 voluntary and community groups that support the prevention approach. The umbrella organization, Voluntary Action Rotherham has a contract worth £500,000 to allocate to voluntary and community organisations that are providing activities as part of the social prescribing programme. Their director is an active member of the Place Board and ensures that the voice of the voluntary and community sector is heard at strategic level and is recognised as an equal partner in achieving the vision. This includes expanding social prescribing for those at risk of hospitalisation and for mental health clients.
Summary headlines from evaluation by Sheffield Hallam University
- The analysis identified an overall trend that points to reductions in service users' demand for urgent care interventions after they had been referred to Social Prescribing
- Analysis of wellbeing outcome data showed that, after three to four months, 82% of service users, regardless of age or gender, had experienced a positive change
- The estimated total NHS costs avoided between 2012-15 were more than half a million pounds: an initial return on investment of 43 pence for each pound (£1) invested
Healthy Conversations on alcohol use, smoking cessation, healthy diet, physical activity and Making Every Contact Count (MECC) are two public health interventions that can create positive change by encouraging small sustained lifestyle changes to improve outcomes. Both methods are being adopted by frontline staff across health and social care teams. To date 89 staff across the council and partner organisations have been trained to be able to deliver MECC to their teams.
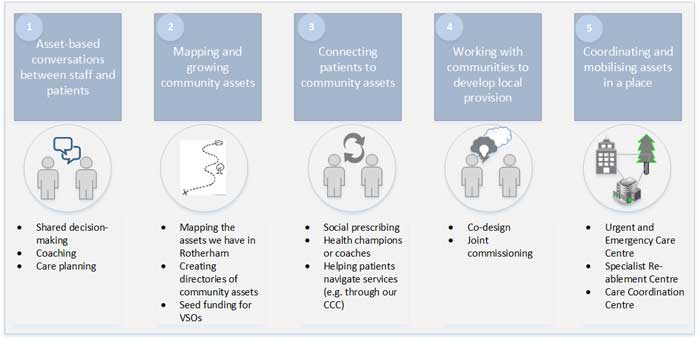
Rotherham has adopted a life course and asset-based approach, which recognizes the crucial role that individuals, families and communities can play in improving health and wellbeing which is presented pictorially below:
This approach is described in the Health and Wellbeing Strategy as an understanding that multiple factors including biological, social, psychological, geographic, and economic, shape health over the life course, and placing people’s skills, networks and community resources alongside their needs contribute to improving health outcomes. This strategic approach is translated into action in the local Place Plan.
Rolling out our integrated locality model – the ‘village’ pilot
The ‘village’ pilot was established in 2016 to develop and test a model based on a multi-professional team delivering health and social care to a general practice population in a single seamless pathway. The client receives co-ordinated care from a single case management plan and lead professional. The multi-professional team brings together primary and secondary care, social care, mental health, community services and the voluntary sector, reducing the reliance on the acute sector. A phased implementation for the six other localities is planned this year which will also include transformation of the care home sector.
Evaluation of this pilot showed evidence of a positive impact on emergency admissions from locality working: all Rotherham localities saw an increase in emergency admissions between 2015/16 to 2016/17, whilst ‘the village’ saw a 2.1% decrease. There were also reductions in hospital length of stay for the village patients as well as the number who were able to safely return home immediately following discharge. All of these positive outcomes showed the benefits of integrated working in ‘the village’ over the other localities.
One interesting feature is that the joint care-planning and support addresses both the psychological and physical needs of an individual recognising the huge overlap between mental and physical wellbeing. In this approach, service integration is a vehicle to deliver parity of esteem.
Integrated urgent and emergency care centre
A new state of the art, Urgent and Emergency Care Centre was successfully opened in July 2017, delivering an innovative integrated model to improve co-ordination and delivery of urgent care provision. The centre is Rotherham’s 24/7 single point of access and triage for urgent and emergency care cases. It uses an innovative multi-disciplinary approach with teams working together within a single unit. The centre seamlessly integrates GPs, ED consultants and nurses as well as mental health teams and care coordination teams. It also accommodates the GP Out-of-Hours service and coordinates all out of hours health care services from a single facility.
Development of a 24/7 single point of access
The centre provides a central point of access for health professionals and patients into hospital and community based urgent care services. An initial assessment is carried out to determine the most appropriate level of care needed and to deploy the right team. The centre has helped to reduce hospital attendances and ensure the most appropriate community services are accessed. The aim is to expand the scope to include mental health and voluntary and social care provision and these services are being considered for consolidation during 2018/19.
Developing a ‘home first’ approach
Plans are being developed in relation to intermediate care and reablement, acknowledging that the current system was not fit for purpose: with complex, fragmented discharge pathways and an over reliance on beds. In response to this the Urgent and Community Care Transformation Group of the Place Plan are developing small scale pathway pilots to support patients to remain at home, or have home as the principle destination following a hospital admission. This will create a new way of working that requires a change of culture across the system from providing beds, to people remaining in their community, supported by their locality team.
Shared systems
The Rotherham Health Record is an electronic system for sharing health and care information in a secure way with health and care staff who provide care. The system gives them access to the most up-to-date information so that they can provide better and quicker care.
Health and care professionals, including doctors and nurses, are able to see a summary of existing records – such as those held by a GP, hospital or social care provider – to allow them to make the right decisions and ensuring people only have to tell their story once.
This system was already used by Rotherham Hospital (acute and community), and has been rolled out to the Rotherham Hospice and some GP practices. An information sharing agreement has been agreed which will enable Rotherham, Doncaster and South Humber NHS Trust and the Council’s Adult Social Care to come on board in 2018/19.
Workforce
As part of the programme to transform the care home sector, it has been acknowledged that social care staff may be uncomfortable in managing a resident who is frail and experiencing deterioration in their health due to an infection or dehydration. The aim is to upskill staff in assessment and practical skills to manage residents in the setting rather than transferring them to another level of care and also to facilitate earlier discharge from hospital.
Joint senior appointments covering Adults, Children’s, Mental Health and Learning Disciplinary services have been made between between the Council and CCG. The joint posts ensure joined up thinking and help avoid unintended consequences for partners as services are transformed. The joint posts are responsible for implementing the Place Plan so conflict is often avoided. Time management is a challenge for the joint posts as short term issues arise and the joint posts are actively encouraged to prioritise the implementation of the place plan.
Communications
The approach to communications focuses on informing, sharing, listening and responding to the people of Rotherham. The communications and engagement group, including communications leads from all partners, meets on a regular basis to develop specific communication and engagement activity, including local media. Communication is carried out in a simple and easy to understand way, which demonstrates how local services are being transformed. The inclusive approach to communication with key individuals and groups include:
- Proactively and effectively communicating the vision, priorities and achievements
- Developing two-way communication opportunities where the partnership shares news, listens and responds and are visible to local people
An infographic and animation has been used as a key tool in articulating how the priorities are closely interlinked to deliver better, more accessible services in the coming years. An example of a recent campaign is the launch of a ‘Five Ways to Wellbeing’, utilising a variety of promotional materials to raise awareness of the importance of good mental health. Each partner organisation within the Integrated Care Partnership will promote one of the five themes throughout 2018/19.
Next steps
The Integrated Care Partnership is working well but members acknowledge that there are more partners to draw in in order to tackle some of the wider determinants of health, including housing, leisure, and environment. There is a need to look at the experience of people with learning disabilities and autism. Joint posts are seen to be the way forward for both commissioners and providers and there is even talk of whole system posts. Joint budgets where it makes sense to do so and joint organisational development are key priorities going forward. What is clear is that the strength of relationships between senior leaders and shared commitment to improve health and care outcomes for the Rotherham population are making a difference and will continue to do so.
Download Integrating health and social care: Rotherham case study