Executive summary
The Chancellor is conducting the 2020 Comprehensive Spending Review (CSR) in unprecedented conditions. As a nation, we are dealing with the impact of the COVID-19 pandemic on people, the economy and public finances. This is alongside the transitional period, following the UK’s exit from the European Union, coming to an end on 31 December.
As we start to look forward, the CSR is a once in a generation opportunity to shape the direction of this country for years to come. We need a collective effort to rebuild our economy, get people back to work, level up the inequalities some face and create new hope in our communities. Responding to the significant economic challenges ahead requires renewed joint endeavour between local and national government as equal partners.
No other body understands local areas better than councils. The highly-valued services we deliver – including public health, adult social care, children’s services, homelessness support, provision for the vulnerable and those in financial hardship – have been absolutely crucial to the initial COVID-19 response by protecting lives and livelihoods. Councils are ambitious for our communities now and into the future, and always stand ready with local solutions to the national challenges we face.
The effective delivery of this next phase will depend on all agencies working in partnership at the local level, and councils are best placed to convene this work. Different areas of the country will require a unique and coordinated response in the coming months and years. Local leaders stand ready to bring government departments and agencies together to deliver locally determined and accountable outcomes. This will allow us to address the biggest public service challenges that have held our nation back for so long, such as social care, health and skills and employment. Our paper, Re-thinking Local, set out our vision for this new approach to devolution.
Bringing power and resources closer to people is the key to delivering better outcomes for communities, tackling deep set inequalities and building inclusive growth across the country. Councillors and their councils have the democratic mandate, expertise and local insights to change our communities for the better. People both rely on, and are reassured by, their local leaders. The Local Government Association’s (LGA) recent polling shows that 73 per cent of residents trust their local council to make decisions about how services are provided in their local area. With the right powers, sustainable funding, and enhanced flexibilities local government can build on the positives we have achieved in the past few months and ensure our communities prosper for the future.
One only needs to look at how councils responded to COVID-19 in an unprecedented manner, even with pressures growing on increasingly fragile services that supported the most vulnerable, such as children’s services, adult social care, and homelessness support.
Despite these unresolved issues, at a time of national crisis, councils put their local leadership role first. They moved at pace, used innovative approaches and worked flexibly to set up completely new services to support the most vulnerable, reshaped and redesigned services such as waste collection to keep them going virtually unaffected, and were central to the economic support provided to residents and businesses. Central Government and local communities trusted them, and they delivered. Throughout, councils learnt from and supported each other through sector-led improvement.
However, as things stand, many councils are in a precarious financial position. After a decade of reductions in funding and rising demand – from which we seemed to be beginning to emerge –councils, along with the rest of the nation, have faced the impact of the COVID-19 pandemic on their citizens, staff, services and budgets. Estimates by the Institute for Fiscal Studies (IFS) suggest that another £2 billion might be needed this year to meet all the pressures and non-tax income losses that councils have experienced and will experience as a result of COVID-19, but that this could rise to £3.1 billion depending on whether councils’ assumptions about the end of the pandemic are correct. Further funding to cover local tax losses, as well as one-off costs that will be incurred to help local areas recover from the impact of the pandemic, will be required as well.
But we also need to look beyond 2020/21 to the next few years. Councils will continue to face demand pressures on their day-to-day services, some pre-existing, others made more significant by the lasting impact of COVID-19 – all against weaker prospects for income, such as local taxation, fees and charges.
As part of its recent analysis commissioned by the LGA, the IFS estimated that councils face cost pressures of nearly £9 billion by 2023/24 in comparison to the 2019/20 starting point. When considering other pressures set out in its report, such as the fragility of the adult social care provider market and the impact of a future revaluation of pension funds, this could lead to a funding gap of £5.3 billion by 2023/24 even if council tax increases by 2 per cent each year and grants increase in line with inflation.
The IFS is also clear that we are still in a period of great uncertainty, with no allowance made for longer-lasting service demand impacts of COVID-19 to councils. The IFS’s upper estimates of all the pressures outlined above as well as challenges of recovering self-raised income suggest that the funding gap could end up being as high as £9.8 billion by 2023/24.
In addition to putting current services on a sustainable footing, councils need the resources to rebuild and recover on issues such as early intervention, public health, concessionary transport and others. Our submission sets out these further pressures on core funding in more detail.
It is clear that the starting point for a new approach to public services, a joint endeavour with national government, in every part of the country needs to be a re-think of public finances with a multi-year financial settlement which provides local government with certainty over their medium term finances, sufficiency of resources to tackle day-to-day pressures and the lasting impact of COVID-19 on income and costs, and that recognises the benefits of investment directed by those closest to the opportunities for shared prosperity.
To achieve this, the Spending Review will need to move away from the traditional drivers of departmental spending towards a degree of fiscal decentralisation in line with some of the world’s most productive economies. The economic challenges our communities are facing require a bold response – place-based budgets which are in tune with the needs of the local economy. We need to re-think how we fund public services, not try to fit new and bold ideas into old frameworks.
This submission, separated into five distinct chapters, sets out how local government can act as the driver to achieve shared priorities between central and local government. Together, we can strengthen the UK’s economic recovery, level up economic opportunity, tackle social and health inequalities, improve outcomes in public services, achieve net zero carbon emissions and improve the value for money of public spending.
- Overall council funding makes the case for sustainable core funding for local government and enabling councils to bring together budgets of public services across a place to eliminate duplication of effort and drive savings to the public purse. Key proposals in the chapter include:
- A multi-year ‘core’ local government funding settlement which provides sufficient certainty and resources to help councils recover from the impact of COVID-19. Taking the pressures estimated by the IFS together, councils face an estimated a funding gap of £5.3 billion by 2023/24 which could grow to as high as £9.8 billion due to the uncertainty resulting from the continued impact of COVID-19. This gap is already after taking annual 2 per cent council tax increases and inflation-linked growth in grants.
- Our four-point plan to allow councils to deliver further public spending efficiencies by joining up local services in a place and eliminating the fragmentation of funding;
- Our proposals to reform and improve local taxation, as well as using the business rates review as an opportunity to discuss how council funding can be further diversified through other forms of taxation.
- Care and health inequalities builds the argument that services for children and adults, combined with a reinvigorated local public health offer, provide the opportunities to tackle health inequalities, manage the on-going impact of COVID-19 and ensure older and disabled people can access the care and support they need. Getting the support right for those who need it most is essential to minimise the costs of poor health, extreme inequalities and poor outcomes later on. Key proposals in the chapter include:
- Our reiterated commitment to work with the Government to deliver a reformed system for funding adult social care and the principles for the delivery of care and support that should underpin the new funding framework;
- Opportunities to improve the life chances of children and young people by ensuring access to high quality services and support including children’s social care, education and youth services;
- An ambitious four-sided strategy for unleashing investment and improvement in public health services, through the recovery of the public health grant, a Prevention Transformation Fund, place-based council leadership and incentivising behaviours.
- Environment and climate change deals with one of the most important issues facing the world today, highlighting the vital role councils play in tackling it. Key proposals in the chapter include:
- A call for crucial investment to allow councils to help Government achieve its aim for the UK to become a net zero carbon economy in 30 years’ time;
- Measures needed to make sure that the ambitious waste and recycling reforms are introduced in a financially sustainable fashion; and
- Ways to improve our ability to adapt to, and manage, the impacts of climate change, including flooding.
- Economy and ‘levelling up’ focusses on the role councils can play in the economic recovery from COVID-19 and the subsequent recession, in particular through greater devolution and powers to steer resources to local economic priorities. Key proposals include:
- A revamped framework for providing councils with capital infrastructure funding, to match the direction set out in the National Infrastructure Assessment;
- An innovative, devolved approach to make sure that local residents have the right skills to match work opportunities of the future; and
- Tackling economic issues affecting the most vulnerable residents, such as homelessness and the welfare safety net.
- Finally, Great places to live showcases the role councils play in building thriving local areas which can boost the sense of community, connection and pride in a place, which can yield further positive economic benefits. Key proposals include:
- Measures designed to improve the public realm, for example through thriving parks and green spaces,
- Funding, powers and flexibilities to help councils deliver housing that is both affordable and sufficient in numbers; and
- Making sure our communities are safe and well looked-after and can rely on essential regulatory, community safety and emergency services, such as fire and rescue.
Combined together, they present a once-in-a-lifetime opportunity to re-think public spending in a way that is fit for the future, flexible to allow the delivery of local priorities, and empowers councils to deliver on the ambition for our communities that central and local government share.
Overall council funding
A strong and certain financial foundation
1.1 Councils are ambitious for our communities now and into the future, and always stand ready to offer local solutions to the national challenges we face. This includes continuing to deliver for our communities during these unprecedented times, while also boosting local efforts to revive and rebuild the economy. However, they require the right powers, sustainable funding and enhanced financial flexibilities to do so.
1.2 The COVID-19 pandemic is already having a profound impact on the economy. There has been an increase of over two million in Universal Credit claimants, which has also translated into higher demands on council tax support. Meanwhile, the Job Retention Scheme is supporting six million jobs on the basis of the latest data, many of which are likely to be supported until the end of October, at which point the scheme is expected to end.
1.3 The economic impact is having a big effect on public finances – both for the Exchequer through national taxation and local government through local tax income, fees and charges.
1.4 The best possible efforts of councils to spark local recovery will not bear fruit without sufficient funding and a sustainable local government finance system to underpin them all. Councils need confidence in the financial system to be able to act, and this is particularly important if councils are expected to be innovative and invest in local solutions.
1.5 Best value for the use of public resources can only be achieved if councils are able to plan and are placed on a sustainable long-term financial footing.
1.6 Prior to the pandemic, councils had already dealt with a £15 billion reduction to core government funding between 2010 and 2020. While a significant part of this challenge has been met through efficiencies and transforming services, councils still had to ration services such as cultural services, economic development, libraries and others to ensure they could continue to protect vulnerable children, for example.
1.7 In addition, councils were facing a funding gap of £6.5 billion by 2024/25, even under assumptions of sustained council tax increases of 2 per cent each year, fees and charges rising and continuing business rates growth.
1.8 Now, councils are also dealing with the sharp end of the immediate financial impact caused by the extra costs, loss of income and cash flow pressures arising from COVID-19. Savings plans and transformation efforts have been put on hold, further exacerbating this unprecedented impact.
1.9 Work by the IFS has indicated that at least £2 billion is still needed to meet the full financial impact of the pandemic in 2020/21 – with the potential for this to grow to as much as £3.1 billion, before even considering the impact of lost local taxes on 2021/22 and beyond.
1.10 There is still significant uncertainty about future pressures related to the pandemic. For example, at the time of writing COVID-19 caseloads are rising, local lockdowns are expanding and the Government is announcing new national initiatives, such as COVID-19 marshals.
1.11 Therefore it is vital that the Government provides a cast-iron guarantee that the financial challenge facing councils as a result of COVID-19 will be met in full – where needed on an on-going basis and not time-limited – before further recovery measures are even considered, as otherwise they will be built on a barely existing foundation. This includes full compensation for lost income and local tax losses. The latter are covered later in this chapter.
Building a strong financial foundation
1.12 To deal with the impact of the pandemic, councils had to reconfigure their services delivery quickly. A large number of temporary services and structures have been introduced, such as:
- Support hubs, especially with respect to shielding the vulnerable
- Local resilience fora
- Measures for businesses as well as residents struggling to pay council tax
- Other specific local services.
1.13 Other pre-existing services have either seen an increase in the cost base that will be very difficult (and not necessarily desirable) to drive down, or are expected to see a ‘bounce-back’ once the pandemic is over. For example:
- Councils have rightly provided adult social care providers with support to help meet additional COVID-19 costs. However, even when the pandemic is over, care providers will be struggling – they already were before COVID-19 – and anecdotal concerns suggest that increased care home vacancies will mean some providers will struggle to stay sustainable on the current income rates. All this implies that councils will find it very difficult not to make the ‘temporary’ cost uplifts permanent and might need to go further to sustain a functioning market.
- Homelessness support will be expected to operate at the increased intense level. The drive to get 90 per cent of homeless people into accommodation has been a big success but it comes at a large cost and the pressure will be on to keep homeless people supported in accommodation once COVID-19 passes.
- There is anecdotal evidence that demand for children’s social care has reduced during the pandemic. This means that, regretfully, a spike of pent-up demand for support to vulnerable children is likely in the ‘new normal’, especially with the evidence that domestic violence is sadly on the rise.
1.14 All of these issues are covered in greater detail in other chapters of our submission.
1.15 Commissioned by the LGA, the IFS has independently reviewed the future funding outlook for councils prior to the Spending Review, including ‘business as usual’ pressures, cost impacts of the pandemic that might be permanent and the potential long-term impact of the economic changes on local income, such as local taxes, sales, fees and charges.
1.16 As part of its analysis, the IFS estimates that councils face cost pressures of nearly £9 billion by 2023/24 in comparison to the 2019/20 starting point.
1.17 When considering these cost pressures and other ‘business as usual’ pressures set out in their report, such as the fragility of the adult social care provider market and the impact of a future revaluation of pension funds, this could lead to a funding gap of £5.3 billion by 2023/24, even if council tax increases by 2 per cent each year and grants increase in line with inflation.
1.18 The IFS is also clear that we are still in a period of great uncertainty, with no allowance made for longer-lasting cost impacts of COVID-19 to councils. The IFS’s upper estimates of all the pressures outlined above as well as challenges of recovering self-raised income suggest that the funding gap could end up being as high as £9.8 billion by 2023/24.
1.19 The funding gap set out in the table below is calculated on the basis of maintaining the current service levels and quality and only accounts for ‘business as usual’ cost pressures.
1.20 We believe that there are a number of other risks to councils’ financial stability which need to be addressed through additional funding. This includes pre-existing financial shortfalls in concessionary fares funding, persistent overspends in children’s social care and homelessness budgets and future new burdens which can be quantified at this time.
1.21 However, councils are ambitious beyond just managing the current challenging state of local finances and services. A number of quantifiable pressures and issues that need to be solved to improve outcomes for local citizens are outlined throughout our submission. They would also have to be funded through additional core funding. This includes, but is not limited to, reinstating early intervention grant, reforming adult social care pay and others. They are listed in the table below and are collectively worth nearly £3 billion on top of the funding gap above.
1.22 To deliver on the Government’s priorities and ambitions, councils have to build on a stable foundation. Across the submission, we are calling on the Government to provide an additional £10.1 billion in core funding by 2023/24, made up by the £5.3 billion funding gap to sustain 2019/20 service levels (already assuming annual inflationary increases to grants and 2 per cent annual council tax increases), £1.9 billion to deal with other quantifiable pressures to stabilise the sector and £2.9 billion of other core funding requirements to help councils improve their core service offer. These figures are broken down in the table below.
1.23 This is in addition to our proposals where specific revenue and capital funding would be required, such as public health funding. They are covered throughout the submission.
Table 1.1. Core funding requirement for councils: breakdown
|
Element |
Paragraph of submission |
Value, £m (2023/24 in comparison to 2019/20, nominal terms) |
|
IFS - central additional ‘business as usual’ cost pressures estimate |
|
8,698 |
|
IFS – central adult social care provider market pressure estimate |
|
1,690 |
|
IFS – central estimate of potential additional costs due to 2023 pension revaluation |
|
678 |
|
IFS – income growth estimates (includes 2% annual increases in council tax and increases in grants in line with CPI inflation) |
|
(5,805) |
|
Funding gap to retain 2019/20 service levels (in addition to inflation increases to core grant and 2 per cent council tax increases) |
|
5,261 |
|
Other underlying pressures and quantifiable new burdens that require appropriate funding |
|
|
|
Pre-existing persistent children’s social care overspend (2018/19 overspend, uprated for demand and inflation using IFS assumptions) |
|
1,013 |
|
Pre-existing persistent homelessness overspend (2018/19 overspend, uprated for demand and inflation using IFS assumptions) |
|
160 |
|
Meeting the shortfall in concessionary fares funding |
4.104 |
700 |
|
Building Safety Bill new burdens |
5.81 |
22 |
|
Mental Health Act – new burdens |
2.170 – 2.172 |
10 |
|
Total other underlying pressures and quantifiable new burdens |
|
1,905 |
|
Other quantifiable core funding requirements to help councils improve and recover services: |
|
|
|
Reinstating early intervention funding to 2010/11 levels |
2.60 – 2.63 |
1,700 |
|
Reforming adult social care pay to match NHS |
2.34 – 2.35 |
1,000 |
|
Restoring the Social Fund to 2013/14 funding levels |
4.72 |
176 |
|
Local digital infrastructure champions |
4.51 |
30 |
|
Total quantifiable core funding requirements to help councils improve and recover services |
|
2,906 |
1.24 While the list above is extensive, it is important to note that there are also pressures and new burdens identified throughout this submission, the funding of which falls on core council resources and are more difficult to quantify at this time. They are also listed in the table below together with references to specific parts of this submission. These pressures and burdens need to be assessed, funded and kept under review.
| Element | Paragraph of submission |
|---|---|
|
Other unquantified pressures which require a boost to core council funding covered by this submission: |
|
|
Adult social care sleep-in shifts: payment of full NLW pending Supreme Court case |
2.37 – 2.39 |
|
Revenue cost of supported housing |
2.40 – 2.42 |
|
Child protection pressures |
2.64 – 2.67 |
|
Revenue cost of new children’s homes |
2.68 – 2.71 |
|
Boosting mental health services |
2.157 – 2.167 |
|
Revenue cost of low carbon initiatives |
3.16 – 3.18 |
|
Revenue costs of climate adaptation measures |
3.33 – 3.40 |
|
Delivery of local clean air plans |
3.46 – 3.48 |
|
Expansion and maintenance of trees and woodlands |
3.54 – 3.57 |
|
Boosting capacity of trading standards, environmental health and other regulatory and protective functions |
5.23 – 5.30 |
|
Other unquantified new burdens: |
|
|
Liberty protection safeguards |
2.171 |
|
Autism Strategy |
2.43 – 2.51 |
|
Armed Forces Covenant |
2.175 – 2.178 |
|
Environment Bill |
3.10; 3.51 – 3.53 |
|
Planning White Paper |
5.21 |
|
Domestic Abuse Bill |
5.64 – 5.65 |
|
New Protect Duty |
5.76 |
|
New burdens resulting from final EU Exit arrangements |
N/A |
Planning certainty
1.25 With a Spending Review taking place in October at the earliest, councils will have gone through three years of quick-fire, short-term budget setting exercises since 2018. In addition, the 2021/22 financial year was meant to see the culmination of the Fair Funding Review, the move to 75 per cent business rates retention and the business rates revaluation all being implemented from next April. All of these have now been postponed – the revaluation will be introduced from 2023 and the other reforms have no specific time frame.
1.26 Without even considering the impact of the pandemic, such a lack of financial planning information does not allow councils to make meaningful and sustainable decisions. For example, councils might make service cuts which would otherwise not be necessary if they had better information. The risks connected to the long-term impact of COVID-19 on local income make this even more challenging.
1.27 A three-year Spending Review presents an opportunity to draw a line under short-term budgeting and to allow councils to set reliable medium-term financial strategies. To do so, the Government should commit to a three-year local government finance settlement to follow the Comprehensive Spending Review. This should encompass general grant funding, specific grants such as the public health grant and council tax flexibilities.
1.28 The impact of the pandemic has not changed the reality that the way general government grants are distributed between councils remains complex, opaque and out of date. It is not possible to succinctly explain why the funding allocations for different councils are what they are. However, it is also clear that any review of distribution arrangements puts a multi-year local government finance settlement at risk, with an impact on certainty. We are calling on the Government to resume the Fair Funding Review, but with a guarantee that the transitional mechanisms will not only ensure that no councils experience a loss of income but should also protect councils from reductions from the path laid out by a three-year settlement, so that they can plan with confidence. The same provision should apply to any business rates reset.
1.29 Councils had to revisit and revise many of their services to react to the impact of the pandemic and it is yet to be seen how permanent some of those shifts are. This means that, when the Fair Funding Review is relaunched, the Government needs to review progress made to date to ensure that it is still fit for purpose, or flexible enough to deal with any such shifts in council service models. One example could be the council tax adjustment (especially the council tax support and collection rate elements).
1.30 Councils’ confidence in business rates as a reliable income source with a future has reduced. The taxbase is currently eroded and council income is propped up by section 31 grants which would fall away at the next reset. In fact, if COVID-19 reliefs become permanent, business rates retention shares would have to go up significantly just to keep the same level of income with local government, without any roll-in of grants.
1.31 While a call for evidence has been launched, the Government’s fundamental business rates review is in its infancy. The next revaluation of business rates will also be highly controversial regardless of when it happens, which will add to the angst surrounding the tax. To aid certainty, the LGA is calling on the Government to not go ahead with 75 per cent local retention of business rates and only revisit this, if appropriate, after the business rates review concludes.
Efficiency
1.32 It is important to recognise that one of the goals of the 2020 Comprehensive Spending Review is to set a new path towards sustainability of public finances after the impact of COVID-19. This requires looking at how the public sector spends money, and on what priorities.
1.33 Councils have delivered more than their fair share of the burden of putting public finances on a more sustainable footing over the past decade. Our analysis shows that around £15 billion of core central government funding has been taken out of councils’ budgets between 2010 and 2020, a drop approaching 60 per cent in real terms.
1.34 Recent research has brought together evidence of the wider financial and economic impact of council spending. This shows that despite funding reductions, council services and activities have delivered significant financial benefits for other public service providers: reducing the demand for some services and providing more cost-effective alternatives to others.
1.35 Local government stands ready to help Government with the task ahead. However, a task of this magnitude, following the experience of the previous decade, needs a completely different approach which unlocks the capabilities of local government to deliver savings across the public sector, instead of looking at local government budgets as just another budget line.
1.36 The traditional means of delivering efficiencies within local government have been exhausted. LGA work undertaken prior to the pandemic showed that the vast majority of remaining variation in spending between councils on older people’s adult social care and children’s services – the two biggest service areas – was explained by factors outside the control of councils (78 per cent and 71 per cent respectively).
1.37 The need to focus all efforts on tackling the impact of COVID-19 locally has also meant that many savings and transformation programmes aimed at delivering savings this year have had to be postponed or cancelled. The data from the July round of the Ministry of Housing, Communities and Local Government (MHCLG) financial information survey suggests this could be worth around £600 million.
1.38 Therefore, instead of looking inward and risking financial sustainability, councils are ready to help Government deliver further significant efficiencies to the public purse through the following four-point plan:
- A renewed focus on prevention, backed by Government investment. A sure-fire way to address existing and future demand for services such as social care, homelessness support and community safety is to invest in lower cost approaches which help strengthen people, communities and local infrastructure. However, with council budgets stretched, a challenge of this scale needs to be kickstarted with Government investment. Our submission provides a rich set of such investment opportunities.
- Reducing the fragmentation of government funding. Research commissioned for the LGA found that in 2017/18, nearly 250 different grants were provided to local government. Half of these grants were worth £10 million or less nationally. At the same time, these grants are highly specific – 82 per cent of the grants are intended for a specific service area. Around a third of the grants are awarded on a competitive basis and often the small amount of grants means that more is spent by councils on preparing bids than is received back. All of these factors mean that if fragmentation and ringfencing of grants is reduced, the system of local government funding can provide much better value for the same amount of funding.
- Bringing budgets together in a place. The approach to tackling fragmented funding can go much further, by looking beyond just local government funding. We need to allocate money to places and not departmental silos. A shared financial and governance framework will mean that services can better align with local priorities and local duplication of efforts can be eliminated. This Comprehensive Spending Review should place emphasis on communities and place by introducing multi-department place-based budgets, explicitly built around the needs of diverse local communities using equality impact assessments.
- Supporting councils to make local self-financed investments to help delivery of transformation of services with associated savings or generated income. This includes improvements to the general capital funding and borrowing framework and improving the consideration of local impacts of investment through the Green Book. This is covered in more detail later in this chapter.
Workforce and capacity
Recruitment and capacity
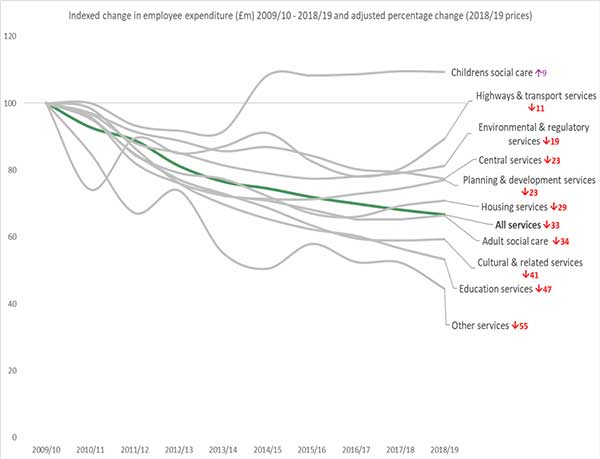
1.39 There have been reductions in most sections of the local government workforce in recent years which has resulted in potential resilience and capacity concerns in light of the foreseeable and unforeseeable demands of events such as COVID-19, EU Transition and the fragility of the social care sector. Reductions in expenditure as shown in the chart below are reflected in reductions in employment. Some of the change reflects the academisation of schools and outsourcing.
1.40 According to the ONS quarterly public service employment survey, in the broadest terms, between Q1 2010 and Q2 2020 the headcount of local government staff fell by around 40 per cent, from 2.1 million to 1.2 million with the full-time equivalent totals for the same periods falling from 1,466,000 to 920,600. This is only in part explained by academisation as the headcount for full time teachers in state-maintained schools in England in 2018/19 was relatively unchanged from 2010/11.
1.41 The only area where staffing has clearly grown over the period is in children’s and family social care where staff levels were 24,890 for the year ending September 2013 increasing to 32,917 by September 2019 (in context, the number of looked after children increased by around 25 per cent in the 10 years to 2019).
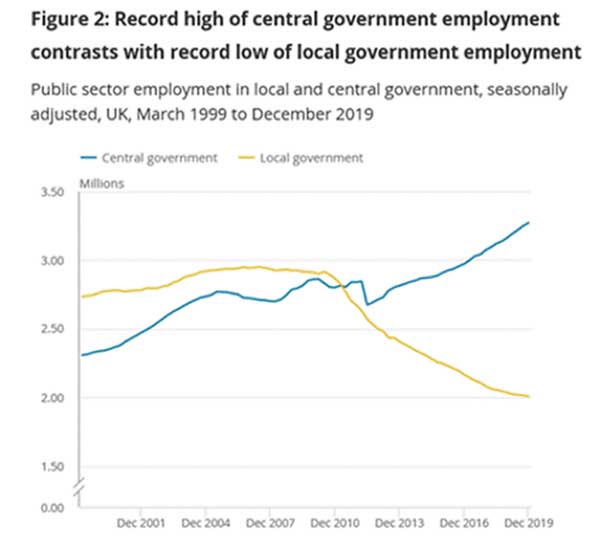
1.42 This contrasts with growth in other public service employment, especially recently, as shown in the next chart.
Chart 1.2. changes in employment, central and local government
1.43 A useful independent analysis of the effects of these reductions on services can be found in a 2018 study by the Institute for Local Government. The study shows for example that 80 per cent of respondent councils had made redundancies as a direct result of austerity and that 90 per cent had reduced services. The survey also examines some of the routes councils adopted to change services. All respondents have redesigned services and the vast majority have used technological solutions.
1.44 However, the limits of innovative change have now been reached in many cases and the experience of the pandemic shows that investment is now needed in both the short and long term to ensure local authorities have the right skills and experience in place to meet these demands effectively. The challenge is threefold:
- in some areas, such as environmental health and social work, there is a shortage of qualified, suitably experienced individuals in these professions;
- in other areas such as building control and engineering, the private sector is able to pay significantly higher salaries than local authorities making recruitment in the sector more difficult.
- There are some bespoke regional issues which need to be dealt with. For example, there are shortages in London in the public health sector.
Returners
1.45 We recognise the importance of enabling people who have had a career break to care for others, or who have lost their jobs, to return to work and bring their skills and experience back into the workplace.
1.46 Further returner programmes should be run in the future to prevent much-needed skills and experience being lost. The Return to Social Work programme has proved of great value during the COVID-19 response and other programmes are due to start for ICT and planning shortly.
1.47 With around £2 million annual funding in the next CSR period, the LGA would repeat these programmes and expand them to other areas where there are challenges in recruitment. For example, environmental health and other regulatory enforcement specialisms have been in high demand during the pandemic response and will continue to be central to renewal.
Registers
1.48 It has been evident during the COVID-19 response that there is a need for increased capacity in some key professions in local government.
1.49 The Social Work Together register (developed by the LGA, DfE and Social Work England) of available, qualified social workers was established early in the response to help meet the urgent demand for children’s social workers. It enables councils to identify potential individuals, who had been provided with necessary refresher training, at short notice.
1.50 So far, around 100 councils have signed up to Social Work Together, and over 1,000 social workers have shared their skills on the online platform and can access relevant training while they wait for councils to contact them about available positions. The social workers are a mix of those on the temporary and permanent registers, meaning they can support both short-term and long-term roles. Councils view the credentials of these individuals for free, avoiding the cost of agency fees.
1.51 Discussions with other government departments suggest an interest for similar projects for other professional groups who are already in high demand and/or will be needed to address EU Exit transition, for example regulatory services including environmental health and trading standards.
1.52 The LGA would like to work with Government to implement a similar model to Social Work Together for these professions to enable local authorities to draw on suitably qualified, available professionals. Each programme has annual costs of around £300,000.
Council pay
1.53 The Government has set a target for the National Living Wage (NLW) to reach two-thirds of median earning by April 2024. The current projection stands at £10.69 per hour by that date (an increase in 19p since the target was announced). The new Local Government Pay Spine was introduced in 2018 to provide a cushion between the lowest local government hourly rate and the NLW. Some differential between NLW and local government rates will need to be maintained, as well the differentials set between spinal column points on the national pay spine.
1.54 Allowing for some headroom to be retained and to accommodate the difficulty in aiming for an as yet unknown target in three years, it is reasonable to set a target for the lowest local government pay rate of £11 per hour by 2024.
1.55 Securing a pay agreement of 2.75 per cent in 2020/21 has helped reduce the cost for the next three years but it remains that case that, in order to have confidence to satisfy the NLW target and retain spinal column differentials in full, significant pay awards will need to be agreed in future years.
Local Government Pension Scheme (LGPS)
1.56 There will be significant additional administrative resources and system changes needed to implement the remedy required by the McCloud age discrimination case. It is estimated that the burden will be similar in nature to the introduction of the reformed 2014 scheme which according to combined annual reports for that year resulted in an increase in administration costs of £9 million per annum.
1.57 The potential impact of McCloud on actual pensions costs is estimated by Government Actuary’s Department to be worth £2.5 billion for the LGPS. This is in addition to the potential annual £600 million cost of the ‘cost cap’ changes to benefits, although there may be a degree of netting off between these two figures.
1.58 Further liability pressures already announced or expected include:
- the Goodwin age discrimination case, with estimated annual costs of £300 million; and
- the equalisation of Guaranteed Minimum Pension which a 2018 Deloitte survey estimated at an average cost of 0.7 per cent of liabilities. For the LGPS this would be just over £2 billion.
1.59 As council employees make up about 75 per cent of the LGPS, the pressures above equate to a risk of approximately £3.6 billion, in addition to £0.7 billion annual pressures from the revaluation of the pension funds which have been set out by the IFS in its recent work.
1.60 There are specific pay and pensions pressures related to fire authorities and teaching staff in schools and they are outlined elsewhere in the submission.
COVID-19 impact on local taxation
1.61 All of business has been affected by the pandemic. The shifts to home working and the enforced business closures have had an effect in the short term, with the long-term implications of COVID-19 not yet apparent.
1.62 Local government has played its part in responding to the pandemic and contributing to measures to help businesses. For example, councils have administered around £10 billion of business rates reliefs and distributed around £11 billion business grants.
1.63 Business rates were due to raise £25.6 billion to contribute towards local government services in 2020/21, both through retained business rates and amounts redistributed through the central share. That accounts for around a quarter of local government revenue spending, or up to 40 per cent if grants to education and the police (which are ringfenced or service-specific) are removed.
1.64 Following the measures announced in March 2020, 40 per cent of business rates in 2020/21 is being covered by retail reliefs (around £10 billion). However, business rates collection is likely to be down even despite the increased reliefs, with current predictions by councils suggesting a £1.6 billion shortfall to the public purse.
1.65 Prior to the pandemic, local authorities set their budgets on the basis of expecting nearly £30 billion of income from council tax, constituting over half of their core spending power. In the context of the current COVID-19 pandemic, the returns to the MHCLG monthly financial information survey for the months of April to July suggest that collection of council tax, in recent years over 97 per cent, could be reduced by 5 per cent to around 92 per cent.
1.66 It is welcome that the Government has already confirmed that councils will be able to spread the impact of local taxation losses over three years. However, the fact that councils will still have ultimately to cover these losses in the absence of Government funding contributes to the £5.3 billion funding gap in 2023/24 as outlined above. Having to deal with these losses at all will hamper the ambition and efforts of local government to improve services and energise the economy as we recover from the pandemic.
1.67 In its funding gap analysis, the IFS assumed that the impact on councils of the shortfall arising from irrecoverable uncollected local taxation in 2020/21, spread over the three-year CSR period to 2023/24, could amount to £602 million for business rates and £493 million for council tax, after netting off the funding already provided by the council tax hardship fund.
1.68 However, this is only one of the scenarios and is subject to great uncertainty because the COVID-19 pandemic is not yet behind us.
1.69 This uncertainty underlines the importance of the need for Government to guarantee that all local authorities will be compensated in full for all shortfalls in planned non-tax income and local tax revenues. This should include parish councils, which would both aid those councils and help principal councils who carry the liability for uncollected local taxation.
Council tax support
1.70 Local council tax support (LCTS) replaced the nationally determined Council Tax Benefit in 2013. This support has been increasingly withdrawn for working age residents. The Institute for Fiscal Studies found in 2019 that the most common level of minimum payment for working age recipients is 20 per cent – adopted by almost a quarter of councils. Another fifth have minimum payments of over 20 per cent.
1.71 One particular reason for this shift is that the central resources to support this have fallen by an estimated £2 billion since 2013/14 at the same time as councils were not able to vary the amount received by pensioners.
1.72 The number of council tax support recipients is rising sharply. Figures for the first quarter of 2020/21 reveals that over 2.5 million working age people across England claimed a discount on their council tax between April and June. That was an increase of 9 per cent from the same quarter in 2019, and the highest number for any quarter since records began in 2015-16. This is expected to be even sharper over the summer due to the continuing impact of COVID-19. The number of claimants may continue to rise in future years due to the knock-on economic impacts.
1.73 Work commissioned by the LGA from LG Futures estimated that the cost of the increased claimant numbers of LCTS due to COVID-19 could be £586 million in 2020/21 alone.
1.74 However, it remains to be seen whether the impact on LCTS costs in 2020/21:
- represents the highest point of the loss or, due to ongoing economic factors (i.e. longer term unemployment / recession), whether this cost will continue to rise over the forthcoming years;
- rises to a high point in 2021/22, as the full year effect of COVID-19 (post furloughing) hits the economy, before continuing to fall; or
- follows a different and unknown trajectory, given the unique circumstances around COVID-19.
1.75 As part of its medium-term outlook analysis, the IFS made a central estimate of the long-term impact on LCTS of the recession of additional costs of £123 million in 2023/24, with an upper estimate of £389 million.
1.76 This estimate is based on data from council returns to MHCLG about the extra LCTS costs in 2020/21 and links to future unemployment rates forecast by the Office for Budget Responsibility.
1.77 However, evidence suggests that council tax benefit claimant numbers were more responsive to unemployment rates during the last recession than councils’ current forecasts for 2020/21 suggest. Taking that past relationship as a proxy, we estimate that the extra cost pressures on LCTS in 2023/24 could actually be worth as much as £570 million, for a total sum impact of nearly £3 billion over the three-year CSR period.
1.78 It is clear therefore that this is another highly uncertain factor that needs to be monitored carefully as it can constitute a significant financial downside that is not captured by central IFS estimates.
1.79 During the last recession, council tax benefit was administered by councils but fully funded by Government in the same way as housing benefit. However, since the transfer to local government in 2013, this is no longer the case and a rise in demand for council tax support of this nature represents a significant unfunded burden.
1.80 If the additional costs of increased demand for council tax support are not fully funded, councils will have to absorb them through reductions in other services or by further cutting the level of council tax support to working age recipients.
1.81 The Government has committed to compensate councils for part of the losses of income from sales, fees and charges and to address the sharing of the impact of council tax and business rates losses between central and local government at the Spending Review. LCTS costs should be part of those considerations and as a minimum include full funding of the whole additional caseload.
Improving local taxation
Council tax reform
1.82 In England, council tax is based on 1991 property values and has not been revalued since then.
1.83 Most discounts and exemptions are fixed nationally. The mandatory single person discount covers almost 32 per cent of dwellings. This discount is not means tested. Other mandatory exemptions apply to students and others. Empty property discounts are discretionary.
1.84 Council tax increases from year to year are constrained centrally, originally through capping and now through centrally imposed limits over which a referendum would have to be held. In recent years the referendum limit has been 2 or 3 per cent with a further 2 or 3 per cent allowed for the Adult Social Care precept for adult social care authorities.
1.85 Council tax is only payable on properties classed by the Valuation Office Agency as dwellings. So, for example, there is no council tax payable on properties not on the list because they are undergoing reconstruction or rebuild. This can result in delays in councils being able to receive income from new or reconstructed dwellings after planning permission is granted, either because they are not built, or they are not valued immediately.
1.86 We would like to work with Government to deliver our three-point plan for making council tax more local:
- The council tax referendum limit needs to be abolished so councils and their communities can decide how local services are paid for, with residents able to democratically hold their council to account through the ballot box. This should apply to all local authority types. Failing that, the Government should consider ways to define the referendum limit which do not reward or penalise councils based on their past decisions. For example, the percentage-based limit could be replaced by a threshold which also allows higher percentage increases to areas with lower council tax levels, similar to the £5 flexibility provided to shire district councils.
- Councils should have the powers to vary council tax discounts to make sure the tax system is fair to everyone according to local circumstances. A prime example is the single person discount, worth 25 per cent of the total bill and applied to all households where there is only one liable occupant regardless of their ability to pay. This discount is worth £3 billion each year.
- To improve the build-out rates of homes with planning permission, councils should be able to charge developers full council tax for every unbuilt development from the point that the original planning permission expires, as opposed to having to wait for the Valuation Office Agency (VOA) to list them following their completion. LGA analysis suggests that over one million homes granted planning permission since 2010 have not yet been built. This is equivalent to three years’ worth of Government’s target number of homes to be delivered each year.
Business rates reform
1.87 As part of the Government’s Business Rates Review, the Government has acknowledged that business rates are an important source of revenue for local government and states that the impact on the local government funding system will be an important consideration in reviewing the tax. It is an important opportunity to take a fresh look at the business rates system as it is being stress-tested by the impact of the pandemic.
1.88 Above all, local government needs a funding system that raises sufficient resources for local priorities in a way that is fair for residents and gives local politicians all the tools they need to be the leaders of their communities. It is therefore important that the tax system, including business rates, provides as much certainty as possible.
1.89 It is widely accepted that taxes should adhere to certain principles of good design. Applied to the local government context, they are:
- Sufficiency – financing for local government services must be sufficient.
- Buoyancy – rises along with economic activity with protection for local government from losses in income given the need to support local government services.
- Fairness – the taxpayer makes a fair contribution and the taxbase is not too narrow.
- Efficient to collect - any tax should be efficient to collect; if the costs of administration and collection of a tax are high then the net yield will be lower than it would be for a more efficient tax.
- Predictability and transparency - income from a tax should be predictable and it should also be relatively straightforward to work out how the tax has been derived.
- Incentive – incentives should be provided to both business and local government.
1.90 Property continues to provide a good basis for a local tax on business. Business rates are efficient to collect and has been relatively predictable and buoyant in recent years. However, the changing nature of business alongside the nature of demand pressures on councils means that we cannot look to business rates to form such a substantial part of local government funding in the future and alternative means of funding councils will be needed instead or as well as a reformed business rates system.
1.91 Many fundamental concepts such as beneficial occupation have been set by case law and not by statute, leading to results which may seem puzzling to the public, such as the fact that large vacant sites may not pay business rates. We have proposed in our response to Tranche One of the Business Rates Review that the Government should bring forward changes in the basis of liability so that more is defined in statute. We continue to support such an approach, and how this is framed should be the subject of a further consultation involving the LGA and councils.
Business rates reliefs, exemptions and avoidance
1.92 The ability to give reliefs, both mandatory and discretionary, is determined by statute, central regulations and case law. The current reliefs system is very heavily weighted towards centrally determined reliefs.
1.93 If local authorities had more discretion over these centrally determined reliefs, they would be able to help local and independent businesses in order to stimulate the local economy. It would also allow councils to incentivise other behaviours that match local and national economic priorities, for example providing reliefs for new or green investments.
1.94 Due to the impact of COVID-19, up to 50 per cent of potential business rates will be covered by centrally determined reliefs in 2020/21 and it might not be possible to achieve the degree of local discretion outlined here immediately. However, the Government should take this opportunity to announce its intention of making most reliefs discretionary with the timetable for implementation to be discussed at a later stage, including how best this can be made fair for business and local government.
1.95 Currently local authorities are statutorily barred from giving discretionary relief to premises occupied by themselves or preceptors. This has become an issue particularly for public conveniences and for market traders. The LGA considers that this statutory bar should be removed.
1.96 The complex framework of business rates exemptions needs to be reviewed. This includes, for example, agricultural exemptions where there are businesses which should normally be rated but just happen to be located on farms. However, we are also aware that the agriculture sector has been hard hit by COVID-19.
1.97 Aggressive business rates avoidance continues to cost councils and central government around £250 million each year. We call for the Government to tighten up on the abuse of reliefs on the same lines as are proposed to come into force in Wales and Scotland in April 2021. Common specific examples of such business rates avoidance are:
- Repeated short term periods of occupation of six weeks or slightly more, resulting in a further period of exemption from empty property rates. This can go together with contrived reoccupation of property, for example by storing boxfiles, in otherwise empty warehouses as evidence of reoccupation.
- Misuse of charitable occupation rules.
- Misuse of insolvency exemptions, through the use of ‘phoenix’ or ‘shell’ companies which trade for a short while and then liquidate.
- Splitting properties in order to qualify for small business rates relief.
- Registering second homes as non-domestic properties to benefit from small business rate relief when the property is not genuinely available for letting. Although the Government consulted on tightening the rules in 2018, no action has been taken.
The business rates multiplier
1.98 Annual uprating of the business rates multiplier is an important source of stability of business rates income. Local government has received compensation for the move from RPI to CPI uprating, as well as new nationally introduced business rates reliefs, during the 2015 Spending Review period and the 2019 Spending Round and it would lose out if this were not to be continued. Around £1.3 billion was paid to local government in this way in 2019/20.
1.99 Any reduction in the buoyancy of business rates, such as including changes in rateable values from constructions, demolitions and alterations in the multiplier calculations at revaluations would be likely to result in a lower multiplier and thus lower income and would have implications for the buoyancy of local government income and business rates retention.
1.100 Local government should be able to set its own business rates multiplier, or at the very least be able to set a multiplier (p in the £) above and below the nationally set multiplier. Local authorities ought to have the power to vary multipliers by property value or property type. This would enable them, for example, to charge a higher multiplier to properties such as warehouses linked to e-commerce in order to support reliefs for other businesses.
Business rates and e-commerce
1.101 Online businesses pose a challenge to traditional businesses and to business rates as a tax. If an activity can be carried out online without the requirement for premises this will reduce the yield of business rates which goes to both central and local government. However, it may lead to other activities that will pay business rates, such as distribution warehouses or businesses which start off online and then decide to open physical premises.
1.102 Taxation should be fair for both physical and online businesses. In January 2020, we launched a report which looked at the potential for an e-commerce levy, which concluded that it is deliverable and offered a number of options on how it could be implemented.
1.103 We welcome the fact that the Government is consulting on proposals for an online levy as part of its business rates review, however the proceeds of such a levy should be retained by local government as a way to diversify the local taxbase and protect against further shifts in the balance between traditional and online retail.
Fiscal devolution
1.104 As outlined earlier in this submission, we strongly believe that delivering further public spending efficiencies will require services delivered by different Government departments to join up locally. To properly unlock the capability of local partners to cooperate, it is important to unlock freedom for public resources to be used more flexibly.
1.105 By opening a conversation about new forms of taxation such as the e-commerce levy and the land value tax, the business rates review provides an opportunity to move in this innovative direction.
1.106 The income to pay for public services at the local level should reflect service demand, should be buoyant and should allow taxpayers to hold decision-makers accountable on expenditure and tax decisions made in their local areas. It should also be sufficiently diversified to guard against shocks and unringfenced to allow for flexible deployment across boundaries of public services and providers, both for capital projects and day-to-day spending.
1.107 Local assignment of taxes can provide areas with incentives to strengthen the local economy as well as create a more diverse funding base, less dependent on central government decisions. It would also allow public sector partners to make collaborative decisions on stewardship of local public funds.
1.108 Recently published research compared levels of fiscal devolution between the UK and three other European nations (the Netherlands, Germany and Switzerland). It found that local governments in these countries have greater revenue raising powers and retain more of their funding locally.
1.109 In addition, econometric analysis drawing on the Organisation for Economic Co-operation and Development (OECD)’s fiscal decentralisation index highlights the extent to which the UK is an international outlier and argues that if the UK moved to the OECD average for tax decentralisation, all regions of England could see a gain in GDP, with an average of 1.79 per cent increase. Currently only 4.9 per cent of taxes in the UK are set locally, whereas the OECD average is 15.1 per cent.
1.110 One way to achieve further fiscal decentralisation would be to assign each local area a proportion of nationally collected taxes paid by citizens in a given area. It would be for local politicians in partnership with local providers to decide on priorities and the allocation of funding. Equalisation would be built into the apportionment formula to account for relative needs, but even so there would be a greater degree of fiscal independence, with areas spending the taxes raised in their communities.
1.111 Assigned taxation is just one option and the right mix of taxes and services should be subject to a full national debate. Some areas will want to think further about options for rebalancing local and national taxation. They will be seeking the freedom to collect different taxes in different ways to support local priorities, or introduce new local levies, such as a tourism tax.
1.112 In the long term, the finance system needs to accommodate the ambition for devolution, which encompasses the full range of public services delivered at the local level. This approach to funding local public services would require a substantial rebalancing of decision-making in England and would put English local government as a whole on the same footing as the devolved administrations.
Capital investment
1.113 Investing in infrastructure through the use of capital spending will be crucial to delivering the social and economic recovery from the pandemic, delivering key government priorities on housing and regeneration, and making the public sector more efficient and able to deliver better value for money while providing key services for citizens.
1.114 The Government has recognised this by prioritising ‘project speed’ and a commitment to the National Infrastructure Strategy. Councils are best placed to deliver on much of this agenda, if given the right financial freedoms, flexibilities and support. The Comprehensive Spending Review is the right place to address this.
1.115 Throughout its five chapters, our submission contains many examples of where councils can play a key role in delivering priorities, such as fixing the nation’s roads and delivering economic regeneration, delivering high speed broadband and high-quality mobile connectivity everywhere, investment in housing (coupled with reform of Right to Buy), schools, transport infrastructure, as well as tackling environmental challenges including reforms to waste and recycling as well as carbon reduction, and investment in digital infrastructure both to improve local areas and enable better service delivery and more efficient ways of working. The future arrangements of the UK Shared Prosperity Fund (UKSPF) are also vital.
1.116 But in order to deliver, councils need the right general financial support and framework.
1.117 Government grant funding of council capital programmes has reduced in recent years. Capital funding in 2018/19, the last year for which outturn figures are published, was £600 million lower than in 2014/15. If 2014/15 levels of grant had been maintained councils would have had an additional £2 billion to invest in local capital projects between 2014/15 and 2018/19.
1.118 Where government capital grant funding is available, it is frequently fragmented and accompanied by bureaucratic and burdensome bidding processes. For example, there are at least 11 different capital funding streams for roads investment alone, each with their own arrangements, rules and allocation processes. Councils have frequently had to consider the risk of investing significant time and revenue resources that cannot be spared into long-winded processes that are not guaranteed to deliver any local benefits. This is something that the Green Book levelling up review should address.
1.119 A further funding freedom can be delivered very simply, and at no cost, by making the flexible use of capital receipts arrangements permanent. Government first introduced this flexibility in 2015 and now extended it to 2022. The Comprehensive Spending Review is the opportunity to make this permanent, adding certainty and removing the need for further review.
Borrowing framework
1.120 Instead of uncertain, diminishing and fragmented government capital funding, councils have been relying on their own resources, and on funding capital through borrowing funded by local sources of revenue under the prudential regime; this has often skewed capital investment into schemes that generate revenue as being the only ones that can be afforded while overall revenue funding has been reducing.
1.121 The prudential borrowing framework enables councils to source capital funding based on what is affordable and prudent, but otherwise free from external restrictions. A major part of that prudential assessment is having sufficient ongoing revenue funds to service the cost of borrowing undertaken.
1.122 The main source of borrowing for councils is the Public Works Loans Board (PWLB). This has largely worked well, although the decision to raise interest rates by 1 per cent across the board in October 2019 has had a major impact on councils. At a stroke this increased significantly the revenue costs of any new borrowing and therefore, of any new capital programmes being planned. In response councils were forced to reconsider the viability of several vital projects including projects to build new housing, investing in infrastructure to enable new housing developments to take place, and regenerating town centres.
1.123 Councils have either delayed investment or, where borrowing has still been undertaken, this has meant increased costs to councils which they have had to pay either to HM Treasury or to private loan providers if they have been used instead. The specific discounted loans schemes announced in the spring budget are helpful, but the overall rate rise needs to be reversed.
1.124 We are concerned that Government plans to change the lending terms for the PWLB by linking restrictions to all borrowing in any one year to individual investment activity undertaken by councils (even if not funded by borrowing) will make it harder for councils to borrow from it to fund priority capital schemes. It will also place PWLB officials in the position of adjudicating decisions that are a matter for elected councillors.
1.125 The problem caused by these practical issues was confirmed in a series of workshops run by HM Treasury over the summer for experts from local government. The outcome of the consultation is likely to be published alongside the spending review and we call on the Government to address this practical problem when framing the new lending terms as well as reversing the interest rate rise announced last October.
Reforming the Green Book
1.126 HM Treasury has been conducting a review of the Green Book - guidance on how to appraise and evaluate policies, projects and programmes - used across Government to assess capital investment. This review was announced in the spring Budget and is seen as central to delivering levelling up.
1.127 The Review has been undertaken by officials and officers from the local government sector have contributed comments to the review team. The outcome of the review and the new Green Book are due to be published before or as part of the Comprehensive Spending Review.
1.128 The announced aim of the review in the Spring Budget is to make sure that government investment spreads opportunity across the UK. It will aim to do this by improving the decision-making process with better information especially around levelling-up, improve public and stakeholder confidence in different parts of the country and embed the right culture and data to develop and appraise policies to support levelling up.
1.129 The review presents an opportunity to change the way the Government views local capital investment and in doing so enable investment to be managed better locally delivering benefits across the board.
1.130 The way in which the Green Book methodology is used should be changed to take better account of local circumstances. At present, the guidance places great value on national financial factors, but in a narrow way. For example, it encourages business cases to be developed in isolation from local strategies and not to consider impacts on local places. It does not encourage local factors and local place-based impacts to be taken into account.
1.131 This has significant implications for levelling up and means that local place shaping factors, that can often have significant local financial and social consequences, are often ignored.
1.132 Consolidation of the current fragmented funding arrangements, particularly when they relate to capital, is clearly the best solution, coupled with greater devolution of decision making to the local authorities.
1.133 However, there are amendments that can be made to the Green Book methodology that can also help. For example, a simple change would be to make a local impact analysis mandatory for all projects reviewed using the Green Book. At present local impact analysis is optional.
Driving efficiencies using investment in digital solutions
1.134 Further capital funding is required to level up digital solutions and opportunities that will improve services, enhance accessibility and connectivity, improve security and deliver efficiency for local authorities through innovation, channel shift to online services and maximising the productivity of the workforce.
1.135 These innovations are numerous and are not exhaustive but could consist of the projects that focus on predictive analytics, artificial intelligence (AI) bots, self-serving initiatives, e-forms, Internet of Things networks, improved CRMs, smart place applications, online resident portals, syncing IT legacy systems and better use of digital platforms.
1.136 In order to have maximum impact the opportunity to develop similar solutions must be made accessible to all councils. The Government should fund councils to enable them to support digital inclusion and closing the digital divide by investing in improving the digital skills of local communities to encourage more people to pursue digitally focused jobs.
1.137 Additional dedicated investment should be made in emerging digital infrastructure and connectivity with councils playing a key role in the development of these networks to shape and strengthen opportunities for residents and businesses as new ways of working become the norm. This will reduce carbon emissions and boost economic viability across the country. Research in this field suggests that a programme of £130 million over four years would help contribute to fixing the digital divide and levelling up the economy through digital skills.
1.138 Over recent years councils have proven they are up to the challenge to develop digital solutions that harness emerging technology, build inclusion and enable connectivity in their localities where further support and investment needs to be made to ensure the momentum developed in response to COVID-19 is maintained and grown.
A long term settlement for local government improvement
1.139 Sector-led improvement (SLI) is an approach put in place by councils and the LGA to support continuous improvement.
1.140 The approach was inaugurated in 2011, providing an alternative to the top-down and bureaucratic national performance framework which it has been estimated cost the government nearly £2 billion a year. In contrast, MHCLG provides annual grant of less than £20 million to support sector-led improvement.
1.141 The approach enables councils to improve themselves, is consistent with the principle of local accountability for results and pays for itself several times over. Verified savings of over £40 million per year are achieved and the exact figure is certain to be significantly higher than this, arising from uncosted efficiencies and indirect benefits.
1.142 There are many advantages to sector-led improvement, not least its flexibility. In the midst of the COVID-19 pandemic, the offer was revised to provide relevant support to councils responding to the crisis and is now also providing tools and materials that will aid councils through the recovery. Throughout lockdown, development work on the climate change and digital security programmes has continued at pace.
1.143 There is also evidence that sector-led improvement reduces the risk of intervention in councils. To date there have been seven statutory government interventions in English local government under the Local Government Act 1999, five during the first 10 years after the Act when statutory inspection was in place and two in the 10 years since Audit Commission inspection was discontinued (Rotherham and Northamptonshire), despite the fact that these last 10 years have been a major financial challenge to councils compared with the previous ten.
1.144 The record of sector-led improvement is impressive, but it could be further enhanced if the grant from MHCLG was awarded on a multi-year basis. As a recent independent review of SLI by Shared Intelligence concludes, the current annual grant settlements drive a short-term focus constraining both the impact of SLI and the sector’s ability to evidence that impact. This is not compatible with the reality that action to influence councils’ effectiveness, improvement and innovation is not a quick fix. The annual cycle also mitigates against securing meaningful sector engagement in shaping the SLI offer.
1.145 A longer-term settlement for sector-led improvement would facilitate a longer-term view of the impact of sector led improvement. This would allow SLI to deliver outcomes planned over a longer timeframe, giving councils the certainty they need that sector led improvement will be there to support them over the next three years.
1.146 We call for a three-year settlement for sector led improvement for councils: £70 million over the course of the spending review period to allow this vital work to continue.
Care and health inequalities
Adult social care
2.1 Social care plays an essential role in supporting people to live the lives they want to lead. Before the COVID-19 pandemic this role was often invisible and a submission to a spending review would have had to champion the value of social care.
2.2 The pandemic has changed this. Social care, and crucially its value to people and wider society, is visible to all like never before. Daily media coverage has shown the public the extraordinary lengths the care workforce has gone to in keeping our loved ones safe and well, often sacrificing time with their own families to do so and always wary of the risks they are exposed to. Politicians from all parties have paid tribute to the workforce and the Government has stated that, as a nation, we are indebted to their selfless dedication.
2.3 In just a few short months, the pandemic has revealed to the public at large both the strengths and value of social care, and its many challenges.
2.4 Even before the pandemic, adult social care was under significant financial pressure.
- The squeeze on council budgets has resulted in some adult social care providers being in a perilous state. The IFS has estimated that the pressure on the provider market, resulting from councils paying less than a sustainable rate on commissioned services, is worth £1.34 billion on the basis of most recent data. Over time, if unaddressed this can grow to as high as £1.7 billion due to demand and inflation pressures. This is in line with our past analysis.
- LGA analysis before the pandemic showed that adult social care costs were projected to increase by £1.3 billion each year from 2019/20 to 2024/25 simply to maintain 2019/20 levels of access and quality, but factoring in demand and inflationary pressures, such as the NLW. This included demand pressures for both older and younger adult cohorts. IFS analysis suggests a similar estimate for annual cost pressures.
- Councils received 1.91 million requests for support from new clients in 2018/19, up from 1.84 million requests in 2017/18. Age UK estimates that there are 1.4 million older people who do not receive the help they need.
2.5 The legacy of COVID-19 for social care – and most importantly the people who use social care services – must therefore be a reset, not simply a restart.
2.6 This impetus should spur our thinking around long-term reform of care and support, which we have always said should be built on cross-party cooperation. We are committed to working with Government and all parts of the social care world – particularly those with lived experience – on a way forward that is informed by the many valuable lessons from the pandemic on the role and value of social care in all our lives.
2.7 The Comprehensive Spending Review provides a crucial opportunity to begin that process. It must act on three main fronts:
- provide additional funding to shore up social care ahead of winter and a likely second wave of the virus, with a look to this continuing in future years;
- provide additional funding for the medium term to help address the long-standing challenges that have faced social care, many of which have been exacerbated by the pandemic; and
- use the above funding as a ‘down-payment on reform’ and to pave the way for changes that will finally put the funding of social care on a sustainable footing for the long-term.
2.8 Councils, supported by the LGA, are uniquely placed to help bring about further improvements in adult social care. We have the relationships – both locally and nationally – with partners across health, housing, the voluntary and community sector (VCS) and providers, that are required to drive social care forward and deliver the changes we all know are needed. When councils have been funded to do things, such as commission additional services and implement rapid discharge arrangements to free up beds for COVID-19 patients, they have delivered.
2.9 Councils’ track record on delivery is a strong starting point for assuring the Government that any additional investment in social care will be well used. But we recognise and accept that significant increases in funding, such as we are calling for, would likely require even greater assurance that funding was being used in the right way. Additionally, the experience of the pandemic has highlighted some of the challenges involved in securing effective national oversight of what is an inherently local public service. The LGA is committed to working with the Government to consider how best to develop a clearer national ‘line of sight’ that still remains compatible with the principles of localism and sector-led improvement. The Care Act achieves this in legislative terms, providing a national legal framework for care and support that is locally delivered and expressed. Now is the time to develop a comparable arrangement for oversight.
Bolstering adult social care’s immediate resilience
2.10 The experience of the last few months has demonstrated, without question, that social care will need additional investment to ensure its resilience heading into winter and a potential second wave of the virus. Only by providing social care with the funding that it needs can continuity be secured for older and disabled people and their family and friends providing unpaid care. Of critical importance is ensuring the provider sector is financially resilient.
2.11 Amidst considerable pressures, councils have worked tirelessly – both before and during the pandemic – to maximise all available funding to best shape, commission and deliver services in such a way that supports people to live the lives they want to lead. This work also continues to help reduce pressure on the NHS and councils’ efforts in recent years should be seen as a foundation for future activity that is centred on supporting people of all ages and with a range of different conditions to live their best lives.
2.12 Since the outbreak of COVID-19, the LGA and national provider bodies have worked closely and constructively together to understand the additional costs facing providers as a result of the pandemic and how best to mitigate them. It is clear that councils are prioritising adult social care in respect of the emergency funding that has been made available to them, with nearly 40 per cent of the funding used for this purpose.
2.13 However, it is important to note that £4.3 billion of funding provided by Government so far, to tackle the cost impact of COVID-19, is intended to cover all council service areas. In addition, this is insufficient in comparison to the overall projected £5 billion COVID-19 cost pressure reported by councils for 2020/21, before even considering lost income.
2.14 The Government has already announced an extra £300 million for the NHS to help prepare for upcoming winter pressures. It is vital that adult social care is also supported. The extension of the Infection Control Fund through winter with an additional £546 million and the Government’s commitment to supply care homes with PPE at no cost are therefore very welcome.
2.15 However, the challenges facing adult social care in the short-term extend beyond infection control. It is essential that funding at this critical time is therefore kept under close review.
Tackling pre-pandemic challenges over the medium term
2.16 While there are many excellent and innovative examples of good practice, the fact that funding available to councils has not kept pace with demand has inevitably curtailed councils’ ability to extend their reach. Consequently, investment in preventative services remains low, the provider market remains fragile, the workforce faces significant recruitment and retention challenges and unmet and under-met need remains a serious issue.
2.17 While much of the media focus on social care during the pandemic has understandably been on older people, it is essential to remember that the number of working age adults requiring support is just as important. In 2018/19, requests for support for working age adults rose by more than 70,000 from 2017/18 to 1.9 million. There was a bigger percentage increase in requests from working age adults (5.1 per cent) from the previous year compared to requests from older people (3.3 per cent). The Association of Directors of Adult Social Services (ADASS) budget survey from 2019 also shows that services for working age adults account for 58 per cent of the demographic pressures on social care budgets, compared to 42 per cent for older people.
2.18 Addressing medium-term pressures on adult social care by meeting the funding gap facing councils, as set out in Chapter 1 of our submission, would help manage consequences of the fragile state of funding for adult social care already seen prior to the pandemic:
- Quality: the latest Care Quality Commission’s (CQC) annual ‘State of Care’ report shows that quality levels in adult social care have been maintained, with 84 per cent of services rated either ‘good’ or ‘outstanding’ (up from 82 per cent last year). However, the report also highlights that access to services is challenging. For instance, some people eligible for homecare have struggled to access support because of a lack of services or a long waiting time.
- Workforce: the aforementioned CQC report also highlights concerns with the social care workforce, with care workers reporting 'chaotic and unorganised shift patterns, at times without breaks, causing many to feel dissatisfied, stressed and undervalued'. If the workforce grows proportionally to the number of people aged 75 and over in the population, then a 50 per cent increase (800,000 new jobs) will be required by 2035. Adult social care pay and conditions are discussed in more detail in the ‘Specific and specialist adult social care issues’ section below.
- Unpaid carers: research by Carers UK shows that carers who care for more than 50 hours a week report poorer health. One in four report bad or very bad physical health and 29 per cent report bad or very bad mental health. Eighty one per cent of all carers report feeling lonely and isolated as a result of their caring role. There is emerging evidence that COVID-19 has exacerbated this, with carers being more reluctant to admit care workers into their homes and with informal services, such as day services, not being available. Young carers encounter particular challenges – for example, they have significantly lower levels of attainment at GCSE level and are more likely to not be in education, employment or training.
- Providers: last year’s ADASS budget survey showed that 75 per cent of councils (up from 66 per cent last year), reported that providers in their area had closed, ceased trading or handed back publicly-funded contracts in the last six months, affecting nearly 12,000 people. Provider organisations have also been expressing concerns about the viability of many of their members. COVID-19 will of course exacerbate the pressures facing providers, particularly in care homes as occupancy rates fall. For instance, an August 2020 survey of 256 care homes by the National Care Association revealed occupancy levels of 81 per cent; this compares with 92 per cent in June last year. Further, research by Knight Frank suggests it is the smaller independent care homes (eg the 6,500 care homes with 40 or fewer beds) that are most at risk as they do not have the scale of larger operators to deal with reduced occupancy levels. Many smaller and sometimes less resilient providers offer the bespoke community-based support that government policy encourages because of the better outcomes it delivers for people.
- Unmet and under-met need: councils received 1.91 million requests for support from new clients in 2018/19, up from 1.84 million requests in 2017/18. In 2018/19 there were more than 8,000 more working-age adults receiving long-term support compared to 2015/16, although the number of older adults receiving long-term support over the same period has fallen by more than 40,000. Age UK estimates that there are 1.4 million older people who do not receive the help they need. This is a significant issue, with the LGA estimating that £6 billion will be required to address unmet need across all adult social care cohorts. Furthermore, this is not purely an issue of unmet need, but also under-met need. Again, this is notoriously difficult to measures but there are undoubtedly people who receive some support but not enough to fully meet the Care Act objective of ‘promoting wellbeing’. This of course increases pressure on unpaid carers and reduces social care’s ability to help mitigate demand pressures facing the NHS.
- Prevention: the aforementioned ADASS budget survey also shows that less than £1 in every £10 spent on adult social care is being spent on prevention. Given the important role prevention plays in increasing people’s independence, reducing the need for more costly care and achieving savings, this further highlights the reality that councils do not have the funding they need to meet all their statutory duties and are having to prioritise those people with the highest level of immediate needs. With appropriate funding, councils could invest in transforming adult social care with a focus on prevention, reablement, assistive technology and supported or adapted housing.
- Supporting the NHS: We support the NHS Long Term Plan strategy which highlights the importance of primary, community and mental health services. However, a recent report by the National Audit Office (NAO) on the financial management and sustainability of the NHS notes that ongoing pressures in social care provision presented challenges for NHS services in terms of efforts to reduce demand. The report also notes that, local NHS bodies remain concerned that without a long-term funding settlement for social care, it will be very difficult to deliver the objectives set out in the NHS Long Term Plan.
2.19 As more medium-term funding is made available, we need to engage with people who need support to understand how it can be used to help drive a more concerted effort to think differently about the way social care is provided, utilising innovative approaches such as micro-enterprises, the wide range of communities’ different assets, mutual aid, and innovative housing arrangements in supporting people, to name a few examples. These solutions feel more ‘human’ and, for many, preferable to some of the more traditional services on offer.
Long-term reform
2.20 Even in the most difficult and restrictive of circumstances, adult social care has been at the forefront of keeping people safe and well in different settings across the country. The huge range of activity across organisations to support people has also been notable for being an inherently local response, with councils playing an important leading and coordinating role. In this way, social care has also shown itself not as an inevitable end point on a journey toward a service or services, but as the way in which people are supported to continue their own personal journey in life. The extent to which social care is framed in this way in the weeks ahead will be an indicator of the scale of the Government’s reform ambitions.
2.21 The Government promised plans for such reforms in January and it appears these plans will be delayed again until next year. This is extremely disappointing, and we urge the Government to publish their plans at the earliest opportunity. As many commentators have said, the options for reform are – ultimately – limited and finite and include implementation of Part 2 of the Care Act. These Dilnot reforms would help tackle one dimension of the ‘fairness’ issue, but they do not deliver extra resources to meet unmet or under-met need or realise the legislation’s ambition on prevention.
2.22 Maximising the potential of the growing focus on care and support requires action on several fronts. Now more than ever, we need to recognise that the funding model for social care has held care – and therefore, people – back for too long.
2.23 Such considerations need to be part of the thinking about longer-term reform, the time for which must surely have now come. Everyone needs to be heard in that debate, particularly people with lived experience of care and support, and it cannot be defined within a narrow scope of protecting people from having to sell their home to pay for care. Of course, this is one important aspect of ‘fairness’ that sits at the heart of the debate about the future of care. But it is by no means the only one. Reform needs to consider the bigger picture and the role social care can and should play in helping to support individual and community resilience, wellbeing and independence.
2.24 Through our 2018 green paper, The lives we want to lead, and subsequent publications, the LGA has been making the case for meaningful and lasting reform.
2.25 Most recently, we developed a set of ‘principles for reform’ that more than thirty prominent national organisations acted as signatories to. We firmly believe that if the Government progresses its social care reform agenda in line with these principles, then we stand the best chance of securing the kind of social care system we need for the long-term.
- People first and the value of social care: Whatever emerges post-COVID-19 should be rooted in, and guided by, what works for people, not what works for systems or structures.
- The importance of ‘local’: Social care plays a key role in making connections in our local communities between a wide range of public, private, voluntary and community organisations that all work together in supporting people to be well, safe and independent. Links with housing are particularly important in supporting people to remain independent at home and in their community.
- Workforce: The future requirements of and for the social care workforce should be a far more prominent consideration for Government, both as a standalone priority and in respect of its links with NHS workforce planning. This should include a commitment to a new deal for the care workforce, comprising action on pay, training and development, career progression and professionalisation, and recognition.
- Providers and commissioning: Traditional services (such as residential care, domiciliary care and day centres) will continue to have a role to play in the future. But they need to be part of a much broader local offer including smaller, more bespoke providers, micro-enterprises and wider community assets such as community-owned care, mutual aid and shared lives.
- Health and integration: Health and social care are equally important and decisions and prioritisations about the future of each should reflect that.
- Care and support reform: Protecting a person from having to sell their home to pay for care is certainly one element of the ‘fairness debate’ at the heart of the question about long-term reform. But it is not the only one. The scope of and ambition for social care reform must be far greater, support adults of all ages including unpaid carers, and have at its heart a commitment to the Care Act wellbeing principle and improving people’s choice and control of the care and support they use to live their best life. Progress must be made quickly.
2.26 Any additional funding that is made available to social care, whether in the short or medium term, should not simply be used for ‘more of the same’ and the pre-COVID-19 status quo. Rather, it should be used to help us move to a more person-centred and preventative model of social care that is rooted in supporting people’s wellbeing in line with the Care Act and building resilience in our local public services and communities.
2.27 To enable this, the Government must provide funding that is sufficient to meet additional demands arising from COVID-19, plus pre-existing pressures and reform ambitions.
2.28 This should be made available with as few a set of conditions as possible. At the point of such funding being made available, the Government should indicate how it is intended to protect and enhance social care for the benefit of people who use services and to enable them to live the lives they want to lead in the future.
2.29 The additional funding required to deliver ambitious reform of adult social care is significant. Analysis by the LGA and other stakeholders, compiled as part of our work on the adult social care Green Paper, suggests that:
- Providing care for all older people that need it but currently
- Providing care for all people of working age who need it but currently do not receive it would cost an extra £1.9 billion by 2024/25 beyond meeting business as usual pressures;
- Implementing a care cost cap of £75,000 and an increased means test threshold (Dilnot Phase 2) would cost an extra £4.7 billion in 2024/25 beyond meeting business as usual pressures; and
- Implementing free personal care would cost an extra £6 billion in 2024/25 beyond meeting business as usual pressures.
2.30 This work has led us to previously call on the Government to make the case for increases in Income Tax and/or National Insurance and/or a social care premium. We have been clear that social care needs a risk pooling mechanism; a sharing of the burden amongst the whole population (on a means-tested basis for a degree of progressivity) to ensure nobody faces catastrophic costs, in which the definition of ‘catastrophic’ necessarily varies according to each person’s starting level of assets, with over 80 per cent of lead council members agreeing with the proposal.
2.31 We have also made it clear that building cross-party cooperation is an essential requirement for success. The following additional principles should underpin funding reform:
- Simplicity: is the proposed system clear and easy to understand?
- Transparency: are the costs of care, the raising of funding for those costs and the spending of that funding clear and transparent?
- Risk pooling: do the proposals pool financial risk among the population at large rather than costs being borne solely by individuals requiring care and support?
- Certainty and sustainability: do the proposals raise money for the short, medium and long term?
- Fairness: are the proposals likely to be considered fairer than current arrangements by the public (across a range of dimensions, such as for people who have saved all their lives, protecting housing assets, fairness between generations or fairness in terms of people’s ability to pay)?
- Social contract: would the proposals give the public a clear sense of rights and responsibilities? For example, would the public have a clear sense that, by contributing financially through taxes, charges or other measures, the return would be guaranteed access to services on clear, understood and fair terms?
Specific and specialist adult social care issues
Adult social care pay and conditions
2.32 The coronavirus pandemic has drawn attention to longstanding concerns about pay, terms and conditions in adult social care, especially in comparison with the NHS but also other labour-intensive sectors. There are on-going recruitment and retention problems highlighted in high vacancy and turnover rates that affect service quality. In addition, many staff have uncertain incomes because of the prevalence of zero-hours contracts. The temporary shifts in these patterns due to COVID-19 have highlighted the need to deal with them permanently.
- The estimated turnover rate of directly employed staff working in the adult social care sector was 30.8 per cent in 2019, equivalent to approximately 440,000 leavers over the year.
- It was estimated in 2019 that 7.8 per cent of the roles in adult social care are vacant, equal to approximately 122,000 vacancies at any time.
- In 2019 around a quarter of the workforce (24 per cent) were on a zero-hours contract (370,000 jobs). Almost half (43 per cent) of the domiciliary care workforce were on zero-hours contracts. This proportion was even higher for care workers in domiciliary care services (58 per cent).
2.33 The market-based system of commissioning and provision is well-established and will continue, but it is fragile, with many providers operating at the limits of financial viability, so there is little scope for improving pay and conditions with the current funding structure. In addition, the post-Brexit immigration system announcement has no transitional arrangements for social care and the health and care visa does not cover care workers so dependence on domestic labour will be accelerated and is likely to require higher pay.
2.34 The LGA has long argued that the social care workforce must be developed in a manner equivalent to the NHS as part of a stable, sustainable solution to long-term funding problems and that this must involve “parity of esteem” for social care staff with their NHS colleagues. Any changes to pay and reward must be fully funded by central Government as there is no resource in the sector to meet the demands of this challenge.
2.35 It will be important to assess the best form of comparison with the NHS on basic pay and resulting costs as overall costs could be in the region of £1 billion. It is also the case that some research and deliberation will be needed on coordination of other terms and conditions and the introduction of an effective mechanism for implementation and uprating. To achieve those aims with a reasonable degree of consensus across the sector, we suggest that the Government commission an independent review.
2.36 Notwithstanding this medium-term objective, which we believe could be resolved within the Comprehensive Spending Review term, more urgent attention should be paid to issues around sick pay and the costs of uniforms and DBS checks.
Payment of social care sleep-in shifts
2.37 Councils wholeheartedly support fair pay for care workers. Whatever the outcome of the Unison Appeal against the decision regarding treatment of sleep-in shifts under National Minimum Wage (NMW) regulations, there is a need to ensure that social care staff are paid fairly for their valuable work.
2.38 However, should the Supreme Court uphold the Unison Appeal, which would mean in many cases ‘sleep-in’ time would be subject to NMW regulations, and if providers reduce or cease to offer support as a result of the sleep-ins back-pay tipping them over the edge, there will be a significant impact on the care of vulnerable children and adults and the care workforce. For example, in 2018, one in 10 children’s homes reported being at risk of closure if they were required to cover six years of back pay.
2.39 Estimates suggest that the back-pay liability could amount to £400 million for the adult learning disability sector alone, which councils would struggle to help meet given the already-stretched financial position covered throughout this submission. To remove this uncertainty and risk to providers and councils, the Government should commit to fully funding social care providers and councils for the back pay liabilities and higher ongoing costs they will face from paying the NMW for sleep-in shifts if the Unison Appeal is upheld.
Investing in specialist and adapted housing
2.40 Housing is a key component of health and care and the foundation upon which people can achieve a positive quality of life.
2.41 COVID-19 has further highlighted the importance of people in vulnerable circumstances having a safe and accessible home with the right practical support and care to enable independent and healthy living.
2.42 We have identified the following priorities:
- To accelerate the availability of much-needed supported housing provision for working age adults with additional needs and older people who want to live independently with support, we are calling on government to work with Homes England, housing associations and developers to incentivise building more supported housing across all tenures.
- A sustainable supported housing funding model is needed to ensure that councils can reduce homelessness and help older and other vulnerable people to live well. This means that both the housing and care elements of the cost of supported housing must be adequately funded.
- We need to work together to develop and fully fund a locally-led approach to overseeing the quality and value for money of supported housing, building upon the forthcoming National Statement of Expectations for Supported Housing. Councils are ideally placed to take the lead role because of their wider housing, planning and care responsibilities, and their relationships with local housing associations and other supported housing providers.
- A further increase to the Disabled Facilities Grant would help councils adapt more of the existing housing stock to help older people and disabled adults and children to live independently in their own homes for longer, preventing further pressure on social care and health systems. It is important to focus on adapting and improving existing homes as well as new builds because, for example, over 90 per cent of older people live in mainstream homes and 80 per cent of the homes we will be living in by 2050 are already built.
Autism
2.43 The Government is currently updating the national Autism Strategy which we expect to launch later this year.
2.44 The revised Strategy will rightly centre on supporting people with autism to live ordinary lives in their communities, widening the focus beyond social care and health services. We fully support putting people with autism and their experiences at the heart of the strategy, which is something councils also try to do locally.
2.45 It is important that people with learning disabilities and/or autism can equally access their community safely, with access to opportunities and appropriate support. Particular attention should be given to people with a learning disability where they are at risk of being excluded and/or at risk of falling through gaps in wider community and public sector support. It is also important to recognise that people with learning disabilities and/or autism have a wide range of different needs across diverse communities.
2.46 People with learning disabilities and/or autism should be able to access personalised and joined-up support provided by an appropriately skilled workforce. A range of resourced local support services and a credible local social care, health and education offer are imperative.
2.47 The forthcoming Autism Strategy is an opportunity to further address these issues. The extension of the Strategy to children and young people is an opportunity to give greater focus to the challenges around transition from children’s to adult services.
2.48 However, the strategy needs to recognise that rising demand coupled with further improving diagnostic rates, will place more strain on already stretched budgets of local services, including councils.
2.49 We would like to work with Government on ensuring that the Comprehensive Spending Review includes a commitment to fully fund the ambition of the new Autism Strategy when it is launched. For people with the most complex needs, we would welcome a continued commitment to provide local areas with short-term funding that enables double running to establish robust community support and avoid specialist hospital admissions.
2.50 Councils, through Transforming Care Partnerships, have made progress to ensure that people with learning disabilities and/or autism who display behaviour that challenges and are referred to assessment and treatment centres can be discharged to more appropriate, community based services tailored to meet their needs and support their carers.
2.51 Appropriate community provision is vital to prevent admissions to hospital as well as supporting people to move out of hospital settings, and this requires social care to be fully funded and enough specialised supporting housing. Although numbers of people covered by the Transforming Care Programme are relatively small, they have complex and often multiple needs that require intensive health and care support, often including specialised housing.
Children’s services
Children’s social care
2.52 As the medium- and long-term impacts of the coronavirus pandemic become apparent, more children and their families are likely to need support. In our publication, A Child Centred Recovery, we highlight evidence around the likelihood of increased demand on children’s services as a result of the pandemic – including issues related to domestic abuse, mental health, poverty and substance misuse, the most common reasons for children and families needing help from children’s social care.
2.53 Some children and families will need significant interventions, including child protection plans or even coming into the care system. But for many, they will just need some extra help to get through a difficult period. That could be low level mental health support, sessions with a youth worker, understanding how to support children showing difficult behaviours, or working through parental conflict.
2.54 Unfortunately, the dual impact of significant cuts to council budgets over the last decade and increasing demand for child protection services prior to the pandemic means that these types of universal and early help services have been scaled back or even closed in many areas – despite councils protecting and even increasing children’s social care budgets at the expense of other services. Rising demand for services means that despite budgets for children’s social care rising by more than half a billion pounds in 2018/19 from the previous year, more than eight in 10 councils were still forced to overspend to ensure children were protected.
2.55 Research by the National Audit Office found that spending on preventative children’s services fell from 41 per cent of children’s services budgets in 2010/11 to just 25 per cent in 2017/18. There had been a corresponding rise in spend on child protection services, most notably for looked after children.
2.56 This rise in spend on supporting looked-after children is for a range of reasons. The number and proportion of children has been rising year on year for over a decade. In 2009/10, 64,470 children were in care, or 57 in every 100,000. In 2018/19, that figure was 78,150 or 65 in every 100,000.
2.57 The profile of children coming into care is also changing. The number of teenagers in care rose by 21 per cent between 2012/13 and 2017/18, while the number of 0-5 year olds fell by 15 per cent. The reasons for this are varied, but feedback from councils indicates that child exploitation (both criminal and sexual) and rising numbers of unaccompanied asylum-seeking children is contributing to the increase. Older children are more likely to need accommodation in children’s homes, which are significantly more expensive than foster care, which, in itself, puts additional pressure on children’s service budgets as councils strive to give young people the right care for their needs.
2.58 Councils also report that children requiring support from children’s social care have more complex needs than they did a decade ago, and so need more support to help them thrive. Reasons for this increasing complexity include success elsewhere. For example, impressive medical advances mean that more children are living for longer with complex conditions. We have a responsibility to make sure they get the help they need to live rewarding lives.
2.59 The proportion of young people in custody has plummeted thanks to the dedicated work of councils, the police and their partners. This is a hugely positive outcome for those
young people, but to make sure they remain out of the youth justice system and make good transitions to adulthood, some will need a lot of support from their local children’s services.
2.60 Councils urgently need funding to invest in the preventative services that their local children and families need, so that we can make sure help is available when it’s first needed – not later down the line when the situation has reached crisis point. Analysis by the Early Intervention Foundation found that a failure to intervene early to avoid preventable difficulties for children and young people costs the NHS £3.7 billion per year, and a further £2.7 billion per year for the Department for Work and Pensions (DWP).
2.61 There is clear evidence on the benefits of prevention and early help, including:
- The Troubled Families programme reduced the proportion of children in care and reduced juvenile custodial sentences and convictions;
- Greater coverage of Sure Start centres led to a fall in hospitalisations of children up to the age of 11, saving the NHS £5 million per cohort of children;
- Reducing the attainment gap between disadvantaged pupils and their peers across the country to the same size as in London would deliver an overall economic benefit of around £12 billion over the lifetimes of those young people.
2.62 This evidence highlights the value of early help in not only reducing demand on, and therefore generating savings for, other parts of the public sector, including the NHS and police, but in supporting the levelling-up agenda, giving young people the chance to fulfil their potential in the longer-term and live healthy, happy lives that also enable them to contribute to society as adults.
2.63 We are therefore calling on Government to provide additional funding which could be used to strengthen universal and early help services. The Early Intervention Grant, which covers a wide range of services including children’s centres, information and advice for young people, positive activities for young people, teenage pregnancy and substance misuse services, young offender and crime prevention services, respite care for families and disabled children and other family support services and early years and children’s social care workforce development has fallen from £2.8 billion in 2010/11 to £1.1 billion in 2018/19. Returning to 2010/11 funding levels by providing an extra £1.7 billion would enable councils to reinstate some of these lost services which help tackle and prevent emerging problems and avoid costs escalating later on.
2.64 Funding to meet increased demand for child protection and children in care services is also vital. This includes funding to support the approximately 200,000 children in kinship care, many of whom are outside of the formal system but have similar needs to looked-after children – yet in many cases receive considerably less support.
2.65 Councils have worked hard to protect and increase budgets to support the most vulnerable children, yet increasing demand means that budgets have been unable to keep up, forcing councils to make difficult decisions about where funding will be directed. Further pressure is placed on councils by local circumstances such as levels of deprivation - evidence shows that at least 71 per cent of variation in spending on children’s services is outside of a council’s control.
2.66 We have also seen increasing examples of councils working to support children with very complex needs and needing to spend significant sums to ensure those children are safe and well. Research by the Children’s Commissioner found that children with highly acute needs made up 0.1 per cent of all children supported but accounted for 7 per cent of all children’s services spending, with placements for some children costing in excess of £260,000 per year.
2.67 Councils and the Government have a responsibility to ensure children are safe and well, and wherever possible are able to live with their families. Without additional core funding, councils will find it increasingly difficult to achieve these aims.
Children’s homes
2.68 As outlined above, there is increasing need for children’s homes placements for children in care. This is particularly the case for children with complex or challenging needs, with councils unable to find suitable regulated placements for children resulting in increased use of unregulated placements.
2.69 At the time of writing, the outcome of the recent consultation on the use of unregulated settings was set to be published shortly, which we expect to introduce legislation to make unregulated placements for children under 16 illegal.
2.70 We made clear in our consultation response that unless sufficiency of placements is significantly improved, concerns around the suitability of placements for children and young people will not be addressed. This is particularly urgent given the potential for a rise in the number of children in care as the impact of the pandemic becomes clear.
2.71 Capital funding, particularly if delivered alongside additional core revenue funding, to support the development of new children’s homes would support councils and providers to meet this need. We encourage a focus for this new funding on the development of children’s homes by councils and smaller providers to ensure a breadth of choice when placing children and to help reverse the recent trend of children’s social care provision ownership being increasingly consolidated into a small number of providers without market oversight.
Early education and childcare
2.72 We know that good quality early education can make an enormous difference to children’s lives, including helping to reduce the ‘disadvantage gap’ in children’s education.
2.73 However, we have long raised the issue of funding for early entitlements being insufficient, impacting on the quality of provision and the availability of good support for children with special education needs and disabilities. While high quality provision supports children’s development, low quality produces no benefit or even negative effects and we know that low funding rates result in low pay for childcare workers. This is resulting in a recruitment and retention crisis in the sector, in particular for the well qualified staff who can make the biggest impact on children’s development.
2.74 This situation has been exacerbated by the pandemic. A combination of historic underfunding for early entitlements and the significant drop in parent paid fees as a result of the lockdown means that the financial sustainability of early years providers is a real concern for councils, with a third of providers in deprived areas fearing closure within a year.
2.75 Maintained nursery schools currently receive supplementary funding in recognition of the extra costs they face, for example the requirement to have qualified teachers. They both achieve the highest Ofsted ratings – 63 per cent are outstanding, compared to 20 per cent of all providers on the early years register – and support more children with Special Educational Needs and Disabilities (SEND) than other settings. They are also concentrated in disadvantaged areas which is contrary to the trend for good and outstanding provision to be more likely to be located in the least deprived areas. However, this funding is only guaranteed until the end of this financial year.
2.76 As we look towards recovery, we believe that funding rates for the early entitlements in all settings need to be significantly increased to enable the early years sector to reduce the disadvantage gap and allow all children the opportunity of the best possible start. We must recognise the success of maintained nursery schools and properly resource both these and private, voluntary and independent providers to appropriately pay the qualified staff needed to deliver high quality early education.
2.77 We are also calling for an immediate injection of funding for the early years sector to protect those most at risk of failure, to ensure that every child who wants a place can access one.
Special educational needs and disabilities
2.78 Councils urgently need additional support from the Government to meet the ever-increasing demand for support for children and young people with SEND.
2.79 Department for Education (DfE) figures show that
- there are now over 390,000 children and young people with an Education, Health and Care Plan (EHCP) in England, an increase of 10 per cent or 36,000 in the last 12 months alone;
- there were 53,900 children and young people allocated new EHCPs made during the 2019 calendar year, an increase of 10 per cent compared to 2018; and
- the number of new EHCPs has increased each year since their introduction in 2014.
2.80 This rise in demand in support will not be reversed unless the SEND system is reformed.
2.81 The increased scope of council responsibilities post-16 was the most commonly cited factor contributing to rising demand and costs for councils. Our research has found that the post-16 cohort now accounts for 23 per cent of EHCPs and around 17 per cent of spending. This is an area that will continue to grow as the successive cohorts move through the system.
2.82 Our research has also found that the number of children and young people permanently excluded from school has risen by 67 per cent between 2014 and 2018, although this figure has now stabilised. Once excluded, these pupils are funded by councils, not schools, putting further pressure on the high needs funding block.
2.83 Since 2018, more children with special needs are now being educated in settings other than mainstream schools. Alternative and non-mainstream settings are, by their very nature, more expensive than mainstream provision.
2.84 While only 6 per cent of children and young people with EHCPs are in independent and non-maintained special schools, our research found that these placements account for an average of approximately 14 per cent of expenditure.
2.85 Further research commissioned by the LGA has found that the percentage of councils that are overspending their home-to-school transport budgets has increased from 71 per cent to 83 per cent between 2014/15 and 2017/18. Increasing expenditure is being driven by the costs of providing transport for children with SEND, with expenditure on transport for children with SEND increasing by 13 per cent for pre-16 children and by 68 per cent for post-16. Transport for children and young people with SEND now accounts for 69 per cent of all home-to-school transport expenditure.
2.86 We are pleased that the DfE has recognised the challenges that councils are facing in delivering SEND support, with the allocation of an additional £780 million for high needs budgets in 2020/21, but it is vital that councils have long-term certainty over funding to support children with SEND, including a commitment to write off council’s existing high needs block deficits.
2.87 The Department’s ongoing review of SEND should set out how we can work collectively to increase levels of mainstream inclusion for SEND pupils and place fewer pupils in much more expensive independent and non-maintained special schools, as well as giving councils the powers to hold local partners to account for their work to support SEND children and young people.
Schools capital
2.88 Despite significant reforms to the education system that have reduced the role of councils, our members continue to have a unique responsibility to ensure that there are sufficient school places locally. However, they have few direct powers to create new school places and sometimes have to borrow to make good a shortfall in capital funding for new school buildings that they will not own.
2.89 To date, many new places have been created by expanding existing maintained primary schools, as this is the most cost-effective option. But, councils have no powers to open new maintained schools or to compel academies or free schools to expand to meet demand. As demand for additional places moves to the largely academised secondary sector, councils are concerned that they will not have the powers to meet their statutory duties.
2.90 We are calling on the Government to give councils the powers to open new maintained schools, where that is the local preference. In many areas, councils work closely with academies and free schools to create new places, but where this doesn’t happen, councils need backstop powers to force academies to expand to meet local demand.
2.91 The Government previously commissioned research looking at the effectiveness of the DfE’s capital investment, including spending on schools. This report found that the capital allocation process is complex, time-consuming, expensive and opaque. In most cases, decisions are not based on objective criteria which are consistently applied and do not succeed in targeting money efficiently to where it is needed.
2.92 The James review of education capital was published in 2011 and schools’ funding arrangements have become ever-more complex since then. The Government should look again at the findings of this review and specifically the recommendation that the capital allocation should be determined using objective information on need for pupil places and on the condition of the local estate. At a local level this notional budget should be turned into a light-touch local plan to achieve the overall goals of the investment.
2.93 More recently, in 2017 the National Audit Office found that there are seven main sources of capital funding for schools and that while councils have created a large number of new school places, they face challenges in continuing to meet demand for additional places on time.
2.94 To help councils meet their statutory duty to provide enough school places, we are calling on the Government to replace the existing, fragmented school’s capital funding arrangements with a single, locally held funding pot. Councils, working closely with schools, are ideally placed to hold this capital pot to quickly identify and allocate where funding is most needed.
Teachers’ pay
2.95 Local authorities need confidence that they will be adequately resourced, through the National Funding Formula, to meet the cost of 2021-24 pay awards for teachers.
2.96 In line with existing Government policy, the following pressures will need to be reflected in the schools funding settlement:
- An estimated 17 per cent increase in pay is needed over the next two years to meet the Government’s commitment of a £30,000 starting salary for teachers by 2022.
- Councils have not received any additional funding for pay awards for 3,666 Centrally Employed Teachers (CETs) for the last three years (2018 - 2020). This funding shortfall has contributed to a reduction of 234 CETs since last 2019. For example, CETs in maintained schools providing SEND and music services, require an estimated £4.6 million increase on the CET pay bill for local authorities for this year’s award alone.
2.97 The Teachers’ Pension employer contribution grant provides funding for the increase in the employer contribution rate from 16.48 per cent to 23.68 per cent from 1 September 2019. The grant values were not increased to take into account the 2019 and 2020 pay awards for teachers, this is a significant additional cost for schools. The grant also does not include funding for pay uplifts for teachers centrally employed by local authorities.
Unaccompanied asylum seeking children (UASC)
2.98 Councils have a strong track record in welcoming asylum-seeking children, working with central government, national partners and regional bodies. As well as volunteering to support children resettled in their area, councils also volunteer to support children and young people via the national transfer scheme.
2.99 The need to find sustainably funded long-term solutions has been thrown into sharp relief by the crisis in Kent over the summer. The number of unaccompanied asylum-seeking children reaching the Kent coast via small boats crossing the Channel has been increasing rapidly since the start of the pandemic. The council is struggling to find enough suitable accommodation while stretching the capacity of the workforce, having to take the emergency step of indicating that they were no longer able to support children safely.
2.100 We welcome the consultation on the future of the national transfer scheme to ensure there are sustainable solutions for the support of newly arrived children across the UK and some local authorities have offered support through the National Transfer Scheme.
2.101 However, many councils have continued to raise concerns that the main barrier to participation is the cost of supporting UASC and UASC care leavers. This is not fully covered by the Government, compounded by wider pressures on children services and overall local government funding.
2.102 The Government needs to fully fund the cost of supporting UASC and former UASC leaving care to ensure that local authorities are properly resourced to provide children and young people with the care and support they need. For example:
- A report by East Midlands Councils identifies that the average cost to a council in the region of supporting a former UASC is £16,602 per care leaver per year, compared to the then £10,485 received in Government funding.
- Using data provided by dozens of responding local authorities, a report from the Association of Directors of Children Services (ADCS) indicated that the grant funding provided by the Home Office covers on average 50 per cent of the costs of caring for a UASC.
2.103 Funding has increased since both of these reports were published, but this has not been sufficient to meet the full challenge.
2.104 It is important to note that the ongoing challenges faced by councils in ensuring that the needs of children can be met are not just linked to the grant funding, but also relate to access to therapeutic services, places to learn English, legal advice, and translation services, as well as an effective age assessment, decision making process and sharing the risks around legal challenge.
2.105 We need a conversation across government and with other partners on ensuring access and funding for these and on meeting the true cost of councils’ statutory responsibilities for this group.
Youth justice
2.106 Council youth offending teams (YOTs), the police and their partners have an outstanding track record of working with young people to avoid them coming into the youth justice system. There has been an 85 per cent drop in the number of first-time entrants to the youth justice system over the last decade, and an 83 per cent decrease in the number of children receiving cautions or sentences over the same time.
2.107 However, over that period, the youth justice grant has been cut by half and there is a concern that these reductions are now threatening those successes. For example, Ministry of Justice figures reveal rises in robbery offences by young people over the last two years following long-term falls. It is vital that the grant remains at least at its current level in real terms to ensure youth offending teams can give young offenders the dedicated help they need, while allowing them to continue with the positive work that has delivered substantial reductions in youth crime to date.
2.108 This will be even more important as we recover from the pandemic. Young people who are not in education, employment or training (NEET) or whose families lose work may look to crime to pay the bills, while the Youth Violence Commission has raised concerns about the potential impact of the pandemic on levels of serious violence as a result of poverty, family insecurity and inequality. Properly resourcing YOTs, youth services and children’s social care will help councils to work with young people and families early.
Youth services
2.109 Qualified youth workers and their colleagues across the youth sector will have vital roles to play in the recovery from the coronavirus pandemic, provided they are adequately resourced. Youth services give young people safe spaces to go and trusted relationships with adults that can be the difference between being supported to make positive choices (including knowing where to go for help when it’s needed) and being drawn into negative situations.
2.110 Youth workers will have a particular role to play in supporting young people with the return to school and helping those young people who struggle to find employment. With young people more likely to experience difficulties in finding employment as the country recovers from the pandemic, supporting them to pursue positive paths through this difficult time will be key to avoiding negative outcomes such as long-term unemployment, mental and physical health difficulties or criminal activity further down the line.
2.111 The National Citizen Service (NCS) receives significant central government funding, totalling £1.26 billion between 2016-2020 despite offering only 2-4 weeks of activity for 16-17 year olds. The programme also achieves low participation rates, with 12 per cent of eligible young people took part in 2016. Participation fell for the first time in 2019.
2.112 While we recognise the value of the programme for those who take part and are keen for the NCS to still be available to young people who want to take part, this time-limited programme cannot replace year-round provision for young people of all ages.
2.113 We therefore encourage the Government to devolve some of the funding for the NCS programme to councils to enable them to deliver or commission the services that local young people want and need.
Tackling COVID-19 through local public health systems
2.115 Public health has been at the heart of the local response to COVID-19. Directors of Public Health and their teams have effectively led and coordinated the local health protection response, whilst keeping vital health improvement services such as drug and alcohol and sexual health services running with limited resources. The Comprehensive Spending Review should be used to strengthen local capacity and resources and ensure public health teams can continue to manage local outbreaks effectively and provide the vital public health services which support communities to be healthy and protect the NHS.
Health protection and infection control
2.116 COVID-19 is best understood as a pattern of local outbreaks, rather than a national pandemic with a similar impact in every community. As we move into the next phase, it is important that councils have the capacity and necessary data to play their full part in the national programme, so they can understand where the outbreaks are happening and be able to act quickly to contain them.
2.117 Environmental health, emergency planners, trading standards and public health are just some of the council services whose expertise and experience are crucial to help stop the spread of coronavirus.
2.118 The national arrangements to track and trace coronavirus need to be complemented by making use of existing local knowledge and skills on the ground and the system needs further investment to ensure capacity and resilience in local outbreak control. As the Secretary of State for Health and Social Care said of Directors of Public Health, their local insight and intelligence is a mission-critical part of our response.
2.119 The Government should use this opportunity to ensure the National Institute for Health Protection has the local expertise and resource to ensure their success. This resource is best embedded in local authorities, who have the detailed knowledge of local systems and partners.
2.120 The Government should also use this opportunity to transfer oversight and coordination for local immunisation programmes to Directors of Public Health. Local authority public health teams already have access to community level data on hard to reach areas and can use a wide range of commissioned services and community contacts (such as health visitors, school nurses, drug and alcohol services) to reach the most vulnerable and improve vaccination rates.
Local outbreak control funding
2.121 The NHS Test and Trace Business Plan outlines plans for service development and priorities for the remainder of 2020 with an ambition to support local councils to refine and improve their local outbreak control plans and ensure they have the capacity and capability to implement those plans.
2.122 In this context we believe there is strong case for additional funding both to distribute to councils experiencing outbreaks and to help others put effective prevention in place. This would include costs related to outreach, communications, community anchors, testing site costs, using local laboratories, as well as financial support to enterprises and individuals affected by outbreaks etc.
2.123 We need additional efforts to ensure the national and local partnership for test and trace works effectively – with a focus on the capacity & capability of local expertise that uses council knowledge and the experience of public health teams. This would benefit from an enhanced sector-led improvement programme of support, building on existing cross-sector working and LGA programmes.
A new strategy for local public health
2.124 Every pound invested by Government in council-run services such as public health is helping to relieve pressure on other services like the NHS and the criminal justice system. Just as pressures exist within NHS and social care, pressures are mounting within statutory public health services. Analysis shows that local authority public health funding is three to four times more cost-effective in improving health outcomes than money spent in the NHS.
2.125 The pandemic has shown that investing more in prevention would have led to better outcomes. There is clear evidence that some groups have been disproportionately affected by the virus, with obesity, poor mental health, socio-economic status and ethnicity and disability all increasing the likelihood of COVID-19 being fatal. This is extremely worrying and underlines the need for a strong Government commitment to tackling health inequalities and the need for more council resources and flexibilities to tackle the underlying economic and social causes of ill-health and premature death.
2.126 Public Health England (PHE) found that people from some black, Asian and minority ethnic (BAME) groups are at a significantly higher risk from COVID-19. The Office for National Statistics (ONS) have highlighted the link between the COVID-19 death rate and deprived communities. The Institute for Fiscal Studies (IFS) has reported that evidence is already emerging that the economic repercussions of the crisis are falling disproportionately on young workers, low-income families and women. In order to deliver a robust recovery that reaches everyone, we need to acknowledge and respond to these inequalities.
2.127 Building cohesive communities is a vital part of councils work over the coming weeks. The social impact of the pandemic and the Black Lives Matter movement have shown us the need for councils to build communities where everyone feels valued and equal. Councils must be given the backing and tools to do this – to ensure that everyone can lead a healthy, safe and productive life supported by their community.
2.128 Health should be recognised as an essential part of the economic recovery and vice versa. The LGA report Nobody Left Behind: maximising the health benefits of an inclusive local economy makes clear the link between health and the local economy. The Treasury should lead from the front and hold departments to account for showing the preventative and health implications of their spending plans.
2.129 The following are just some examples showing the need for, and effectiveness of, investing in public health and prevention services.
Reducing the harms of substance misuse
2.130 The number of deaths from drug misuse registered in 2018 increased by 16 per cent to 2,670. This is at the highest level ever.
2.131 The combined benefits of drug and alcohol treatment amount to £2.4 billion every year, resulting in savings in areas such as crime, health and social care.
2.132 According to the National Institute for Clinical Excellence, every £1 spent on smoking cessation saves £10 in future health care costs and health gains.
2.133 With a possible sudden increase in free time, uncertainty, anxiety and stress, we know that some people may become more dependent on drugs and alcohol. This, for some, can tip the scales from managed and recreational use into problematic use and addiction. People with substance misuse problems are disproportionately affected by poor health, including illnesses that would categorise them as ‘extremely clinically vulnerable’, as well as a range of other disadvantages – including homelessness – that may put them at increased risk of contracting and being adversely affected by COVID-19.
2.134 In the longer-term, local authorities are fully committed to work to reduce the harm caused by alcohol and drug misuse but continue to face significant funding challenges which have impacted on their work, both directly and indirectly, to support people accessing drug and alcohol treatment.
2.135 Councils have indicated a desire to maintain and accelerate the recovery focus of drug treatment, particularly for opiate users, but also want to address emerging issues such as new psychoactive substances, (eg legal highs) and addiction to medicines. There is an ambition for closer links with sexual health, criminal justice, and housing and youth services and of integration with family focused initiatives, closer links with GPs, improved coordination on domestic violence, and a strong and consistent link to sexual health – teenage conception and sexually transmitted diseases.
2.136 Commissioning workforces in local authority public health teams have been hit by major reductions in funding which has shrunk the workforce and led to specialist substance use commissioners spreading their time and energy across the whole range of public health, and conversely brought those from other areas of public health into substance use.
Improving sexual health
2.137 Latest figures released by PHE show there were 3,561,548 attendances at sexual health clinics in England in 2018, up 21 per cent on the 2,940,779 attendances in 2013, with no additional funding to support increase in demand and treatment.
2.138 Sexual health, reproductive health and HIV services are facing major disruption due to the impact of COVID-19 and are having to make unprecedented service provision decisions, including temporarily suspending many ‘business as usual’ functions. Sexual health providers are operating phone consultations, posting contraception, sending screening tests and medication to people's homes when needed and seeing patients face to face where necessary.
2.139 Public health teams are very aware to the possibility of serious adverse sexual health, reproductive health and HIV outcomes for the general population, including a rise in unplanned pregnancies, sexually transmitted infections and abortions. With reduced access to essential services, this is already putting considerable additional pressure on primary care and other emergency settings who do not have the capacity or expertise to efficiently manage those presenting with sexual, reproductive health and HIV needs.
Reducing obesity
2.140 The number of people with Type 2 diabetes is expected to increase by a million – from just under four million people in 2017 to almost five million in 2035.
2.141 Research shows that the yearly cost of council funded community-based social care for a severely obese person is nearly double the cost of a person with a healthy BMI, which equates to an extra £423,000 in annual excess social care costs for a typical council. Further research shows that obese people are 25 per cent more likely to be using some form of long-term care in two years’ time, than those with a healthy BMI.
2.142 Tackling obesity through prevention, early intervention and provision of appropriate social care will improve people’s health and wellbeing, pre-empt future health and social care issues, promote independence and reduce the pressures on social care and the NHS and narrow health inequalities.
2.143 Since taking on this responsibility, councils have worked hard to increase participation rates and nearly 1.2 million children were weighed in 2018/19.
Giving children a better start
2.144 Workforce modelling is needed to account for the predicted increased demand for health visiting services (including, additional advice being requested due to the difficulties in accessing GP advice, supporting vulnerable families, domestic violence and abuse, safeguarding and mental health conditions).
2.145 In addition to catching up on routine Healthy Child Programme contacts, we expect to see a surge in activity and demand for support. This will be particularly notable as children return to schools and nurseries and look to support from public health services around infection control.
2.146 Routine childhood immunisation programmes will also need a rigorous and extensive catch up schedule which will require oversight and resources from the Healthy Child Programme teams.
Our four-sided strategy for local public health
2.147 We need to invest in the ongoing resilience of our communities with an assets-based approach which invests in the strengths and capabilities which already exist. Councils need the resources to work in partnership with their VCS to provide low-level support to improve health, wellbeing, participation and resilience. Community resilience and support has been vital in addressing the crisis, but it will also be vital in delivering a meaningful recovery. If public health at a local level is given the parity of esteem it deserves, health inequalities could be levelled, and prevention put at the centre of our future approach.
2.148 We are calling on the Government to work with us to deliver a four-sided strategy to strengthen public health services:
- Sustainable core funding. We know that one thing that marked England out as COVID-19 hit was our poor public health including our high rates of inequalities, of smoking, and of overweight people and obesity. Whilst the pandemic makes it vitally important that prevention is not sidelined, it should be given prominence at all times, with 40 per cent of avoidable deaths as a result of tobacco, obesity, inactivity and alcohol harm. Increases in the public health grant are vital to improve these characteristics.
- Investing in transformation. In order to arm our population against this virus, we will need to turbocharge public health programmes that can reverse chronic conditions such as type 2 diabetes. The Government should work with councils to introduce a new Prevention Transformation Fund, underpinned by a sector-led transformation programme, to help deliver on this shared ambition.
- Strengthening local leadership through devolution. Local authority directors of public health have demonstrated the value of local public health teams being able to respond effectively to the pandemic based on a detailed understanding of their community. As the Secretary of State for Health and Social Care, Matt Hancock said on 18 August, local directors of public health and their teams are the unsung heroes of health protection. ‘Local by default’ is now the approach to addressing public health in the COVID-era. A sector-led transformation programme that can address the issues of obesity, drugs and alcohol abuse, sexual health, 0-19 years and the NHS health check is the best way to sustain this change. It would additionally provide public health transformation assurance.
- Rewiring behavioural incentives and raising revenue. Levies on alcohol, smoking and sugary products can discourage consumption of harmful products while also raising income to help fund other proposals set out in the strategy.
Table 2.1. Details of the four-sided local public health strategy
Sustainable core funding. To match the growth in overall NHS funding as part of the Long Term Plan, the public health grant would have to increase to at least £3.9 billion by 2024/25.
This would allow councils to not only continue to provide current services, but consider expanding other initiatives where financially possible and locally desirable, such as the following:
|
Proposal |
Details |
|
A School Nurse for every school |
School nurses reduce childhood obesity, under 18 conception rates, prevalence of chlamydia, support mental health and can also advise on infection control and support immunisation uptake. Every state secondary school and its cluster of primary schools should have a qualified school nurse with specialist knowledge to provide support around infection control, keeping vulnerable children safe, sexual health, emotional wellbeing, healthy eating and lifestyles. (estimated cost = £106 million) |
|
Expand Health Visiting Workforce |
To return to the target numbers originally set as good practice caseloads in the Health Visiting Implementation plan, an additional 3,000 FTE health visitors would be needed.
(estimated cost - £90 million)
|
|
Perinatal Mental Health Specialists |
In 2016 Health Education England (HEE) recommended that every woman should have access to a specialist health visitor in perinatal and infant mental health.
(estimated cost for every council to have a full-time specialist health visitor in perinatal mental health (1 year) - £5.5 million)
|
|
Investment in Nursing CPD |
In the 2019 Spending Round the Government announced a 3.4 per cent increase in the HEE budget which included an additional £210 million for Continuing Professional Development (CPD) for nurses. HEE has responsibility for development of the public health nursing workforce, however the funding was not made available to this core part of the workforce and undermined the Government’s commitment to integration and prevention in its recent Green Paper and the NHS Long Term Plan.
CPD budgets should be open to all nurses, including specialist community and public health nurses, social care and immunisations nurses. Funding should also be accessible regardless of whether the nurse is directly employed by the NHS, local authority by social and private enterprises.
|
|
Family Hubs |
The Government should work with local authorities to explore the development of health visitors, early years workers and school staff operating out of "children and family hubs” based in or next to schools.
|
|
Shared Outcomes Fund |
Dedicated funding to support drug and alcohol services through a Shared Outcomes Fund. Local government has repeatedly argued that reductions in the public health budget only prove counterproductive to both the public purse and health outcomes. |
|
The Local Government Healthy Weight Programme |
It is widely acknowledged that we need to develop a whole-system approach to reducing child and adult obesity and built on the premise that a healthy life is the responsibility of all of us, schools, neighbourhoods, health professionals, planners, legislators, the food industry and others. Develop a well-funded programme of activity that coordinates action effectively |
|
A rescue package for leisure providers |
Funding to ensure leisure facilities stay open to all communities and recognises their role in the fight against obesity, inactivity and poor mental health, which in turn will help to save the NHS being overburdened in the future. |
|
Active Communities Programme
|
A programme that aims to encourage designers and urban planners to create spaces that encourage physical activity (drawing on the Active Design Guidelines developed in New York City and Amsterdam). The programme should bring examples of healthy planning together, to serve as a source of inspiration and to articulate the principles underpinning healthy planning. Particularly targeted at specific neighbourhoods with the highest levels of need and deprivation. |
|
Investing in transformation |
|
|
Prevention Transformation Fund |
Evidence shows that additional funding for prevention could be highly cost-effective. Local authorities are telling us that they have gone to heroic lengths to deliver more with less and less, but they cannot make the radical upgrade in prevention services asked of them without additional dedicated funding to allow them to make a step change in the types of services they provide and how they provide them. This work stream will advocate for the double-running of new investment in prevention services, alongside current services that public health teams across the country already provide. |
|
Sector-led improvement |
The Prevention Fund should be underpinned and driven by a funded LGA-led transformation programme to strengthen local public health services and address health inequalities with an emphasis on obesity, drugs and alcohol abuse, sexual health, 0-19 years and the NHS health check and providing assurance across local public health. It could be used to improve digital delivery and modernise services e.g. to expand home testing and web-based delivery in sexual health and contraception services. |
|
Strengthening local leadership through devolution |
|
|
Wellbeing in the round – Spending Principle |
As part of its Spending Review, the Government should consider wellbeing in the round, recognising the contribution of different council services and those coordinated by other public sector and voluntary organisations that councils commission. |
|
Section 7a public health services |
The Government should enable joint commissioning of section 7a public health services and to consider devolving responsibilities to local authorities. |
|
Healthy Communities Fund |
Our towns, cities and local communities are playing a growing role in population health improvement and have enormous potential to be health-generating places. Improving population health depends on coordinated action at multiple levels and ensuring that decisions in areas such as housing, employment and transport planning all have a positive impact on health. Community wide co-ordination requires effective leadership, robust governance, and adequate investment.
Additional funding to support healthy communities could include citizen challenges such as that launched by Oklahoma City Mayor Mick Cornett in 2007, for Oklahoma to lose a million pounds in weight together. Less than five years later, the city had accomplished that goal and moved from the list of America’s fattest cities to the list of its fittest cities. The mayor’s program fostered grassroots involvement with people talking about it in schools, workplaces, churches and in the community. An adequately funded nationwide challenge to cities and towns could easily be replicated and create a degree of healthy competition. |
|
Mandation |
Government should strengthen the current requirements surrounding alcohol and drug treatment services. Substance misuse does not respect local authority boundaries and residents in need of support should be able to have access to comprehensive, open access treatment services for substance misuse. There should be an additional mandate to strengthen partnership working through the requirement to have multi agency and stakeholder engagement of local plans and strategies. All new burdens on local authorities through any additional mandation must be properly assessed and fully funded. |
|
Rewiring behavioural incentives and raising revenue |
|
|
Making the case for ‘polluter pays’ |
The Government should make the case for a ‘polluter pays’ principle in the case of mandatory levies on the most health harm producing industries.
|
|
Revenue from alcohol duty is protected to fund treatment services |
Government should protect additional revenue for local authority public health teams to fund alcohol treatment services in a similar way to the Sugar Tax. A similar approach is also used in gambling, where a levy on gambling operators is used to fund research, education and treatment. |
Sport and physical activity
2.149 The Government’s manifesto commitment to invest in the future of sports facilities is a positive step to ensuring that our communities can be active and investing in their future wellbeing. Regular physical activity can reduce the risk of many chronic conditions, including coronary heart disease, stroke, type 2 diabetes, cancer, obesity, mental health problems and musculoskeletal conditions.
2.150 Sport England has commissioned research into the costs of physical inactivity, which showed that NHS providers in England spent more than £900 million in 2009/10 treating people with diseases that could be prevented if more people were physically active.
2.151 The sporting infrastructure is ageing, with Sport England estimating that 63 per cent of main sports halls and 60 per cent of swimming pools are past their expected lifespans or overdue refurbishment.
2.152 This does not mean all of these assets need replacing like for like. Instead, it is vital to work with communities to design the leisure centres, sports pitches, parks and other infrastructure that will best meet their needs and enable them to build activity into their lives. This could also mean realising the potential for new facilities to revitalise the high street, be co-located with other facilities to form wellbeing or community hubs, and ensuring they meet the latest environmental standards for energy efficiency.
2.153 Sport England has been providing effective support and investment in infrastructure, but their funds are oversubscribed with 1,054 bids submitted to a grant fund that could only make 151 grants. Had Sport England been able to fund those bids, it would have unlocked match funding worth at least £540 million from councils and partners. During its operation, the fund typically achieved a 30 per cent reduction in capital build cost and a 40 per cent improvement in efficiency averaging £500,000 per annum per facility.
2.154 We are calling for a strategic investment of £500 million for councils to invest in leisure facilities, pitches, and parks to reduce obesity; ensure a healthier, more active nation in the future; reduce our carbon footprint; and prepare our communities for the inspiration provided by the Commonwealth Games.
2.155 Empowering the public to take greater responsibility for leading a healthy lifestyle is a task that requires a joined-up effort across all public services, not just local government.
2.156 We propose to work with the Government on incentivising the creation of health and wellbeing hubs. These would combine swimming pools, gyms and sports halls, with GP drop-in centres, libraries and police services, to create a one-stop-shop for public services. This would also help tackle the challenges of the current ageing infrastructure, as outlined above.
Mental health
Mental health and wellbeing, including suicide prevention
2.157 Local government’s role in improving and maintaining our residents’ mental wellness across the life course – from childhood to old age – has always been important, but its importance has been further highlighted by the COVID-19 pandemic. In addition to councils’ range of core statutory mental health duties relating to adults and children, they provide and commission services which have a significant impact on the country’s mental wellbeing.
2.158 Councils are central in shaping and delivering a vision which moves us away from focusing on mental ill health to a locally led focus on helping everyone to stay mentally well, providing community support and helping people to continue with their lives. The evidence in support of local government’s mental health and wellbeing role, including early learning from COVID-19, is presented in a recent joint publication with Centre for Mental Health.
2.159 At least half a million more people in the UK may experience mental ill health as a result of the pandemic. Councils are working hard with the NHS, schools, employers and other local partners, especially the VCS, to support the mental health and wellbeing of their residents, including children and young people and will continue to do so as we enter different phases of the pandemic.
2.160 Whilst it is too early to understand the potential impact of COVID-19 on suicide rates, it is worrying that before the pandemic we saw some significant increases, particularly in the male suicide rate and among under-25s generally.
2.161 Mental wellbeing is also crucial to nearly every aspect of recovery planning – from reopening schools, to getting the country safely back to work and dealing with the economic and housing consequences of the pandemic. The mental health impact of COVID-19 will not be experienced equally – people with existing mental health difficulties and risk factors for poor mental health are likely to be affected disproportionately.
2.162 Councils’ actions across the mental health spectrum include continuing to meet statutory responsibilities for adults and children’s mental health needs, supporting the mental wellbeing of frontline staff, bereavement support, suicide prevention, helping residents to stay connected, supporting mental wellbeing in schools, and supporting people who might need additional help such as unpaid carers and new parents.
2.163 Councils also promote mental wellbeing through, for example, safe access to parks, youth services, children’s centres, open spaces, encouraging physical activity and expanding public libraries’ online offer.
2.164 Targeted mental health support will continue to be needed for some groups who have been made increasingly vulnerable by COVID-19 and the lockdown. This includes those experiencing domestic abuse, the digitally excluded, vulnerable children, those who shielded and those with learning disabilities and/or autism. Culturally appropriate responses are also needed given the disproportionate impact on BAME communities.
2.165 As a result, we are calling on the Government to recognise that the mental health and wellbeing recovery is best led locally by councils with their partners and for government departments to adopt a coordinated, all ages, whole family and whole household approach that complements locally-led approaches. This will be necessary to ensure appropriate support for people who have vulnerabilities, including possible future shielding arrangements, and to respond to further local outbreaks.
2.166 Underpinning this must be recurrent local funding for children and adult services to invest in effective mental health services to meet existing, new and unmet demand that has built up during the pandemic. Councils’ public health grant should be increased so that councils can provide locally tailored all ages and whole household mental wellbeing approaches that can promote personal wellbeing and resilience and prevent the escalation of more severe mental health disorders, with the associated impact on NHS capacity, economic recovery and community cohesion. This will be especially important for children and young people and population groups most likely to experience the adverse mental health impacts from COVID-19.
2.167 To further strengthen councils’ suicide prevention work at this critical time we call for the confirmation of funding for year three (2021/22) of the LGA/ADPH suicide prevention sector-led improvement offer to cover public mental health rather than to solely focus on suicide prevention as a more effective approach. This would bring our national approach to supporting councils on suicide prevention in line with local approaches that seek to prevent suicide through addressing the wider social, economic and environmental factors that affect people’s mental wellbeing and can increase the risk of severe mental illness and suicide.
Mental Health Act reform
2.168 The COVID-19 pandemic will likely have many psychological impacts on the population which may have a detrimental effect on the short-, medium- and long-term mental health of some residents. In turn, this may reduce people’s resilience and their ability to cope. Longer term impacts in terms of trauma, grief and distress may exacerbate the burden of mental ill-health in the community long after recovery.
2.169 Professor Sir Simon Wessely’s independent review of mental health legislation acknowledged local government’s significant role in mental health both in terms of its statutory duties under mental health legislation, in particular through the role of Approved Mental Health Professionals (AMHPs) and supporting treatment and recovery in the community.
2.170 We are calling on the Government to fully fund the new burdens from updating the Mental Health Act and implementing the recommendations from the Wessely review. We are also calling for the Government to resource the underlying workforce pressures of AMHPs who are largely employed by councils, as identified in the Department of Health and Social Care’s 2019 National Workforce Plan for Approved Mental Health Professionals. Together, this could cost approximately £100 million over 10 years.
2.171 We are also calling for the Government to fully fund the new burdens across children and adults social care of implementation of the Liberty Protection Safeguards. We have welcomed working with Government on the impact assessment that explores new and revised roles and responsibilities for councils and in scoping a separately funded cross system sector led improvement programme that allows councils and local partners to prepare themselves for implementation by April 2022 effectively.
2.172 The review also had a powerful message about the importance of prevention and early intervention. Care and health systems are interdependent and there is a mutual interest in ensuring that there is a shift in focus to prevention and supporting wellbeing to reduce the need for more intensive or acute mental health services, including detentions under the Mental Health Act.
2.173 Preventing mental health problems requires an understanding that mental health is interwoven with other agendas – including housing, employment, social inclusion, economic development, and safety. Local authorities are uniquely placed to connect all parts of the system. They have the ability to knit together their own strategies to work towards fewer health inequalities and better mental health for all.
2.174 The review makes a positive case for more accessible community-based services, including advocacy, in order to prevent unnecessary detention. Currently local authorities commission or provide a wide range of such services. It is important to recognise that any further increase in such community services would require adequate funding from the Government.
Armed forces covenant
2.175 Councils are fully committed to honouring their commitments under the Armed Forces Covenant and are working hard to support serving personnel and veterans who have been affected by the COVID-19 outbreak.
2.176 However, the scale of the funding challenge facing local government means it is becoming increasingly challenging to maintain the current level of support for the armed forces community.
2.177 Research commissioned by the LGA shows that the Armed Forces Covenant Fund Trust has been vital in enabling councils to get projects off the ground that support their forces communities. Around £6.6 million of funding from the trust’s local government programme has made a difference, but is short-term, with many parts of the country not benefiting.
2.178 Councils need adequate funding so they can support veterans and their families through homelessness prevention, housing, mental health and other services. We are calling on the Government to:
- establish a three-year £12 million Local Armed Forces Covenant fund to further embed and extend local support for the armed forces community; and
- fully fund the new burdens from the statutory duty to have due regard to the Armed Forces Covenant that is being developed by the Ministry of Defence.
Environment and Climate Change
3.1 With at least 230 councils declaring a climate emergency, and nearly two thirds of councils in England aiming to be carbon neutral 20 years before the national target, councils are well placed to support Government to meet its net-zero carbon ambitions by 2050. Since net-zero can only be achieved with decarbonisation happening in every place across the country – that’s every household, community and local economy – it will require local leadership where councils, as democratic organisations can ensure that the benefits are felt by all.
3.2 The Government should work with councils and businesses to establish a national fiscal and policy framework for addressing the climate emergency. This framework should outline responsibilities for the Government nationally – for example, aligning the regulatory system, including the planning system and national tax incentives – and the local responsibilities, together with a commitment to cooperate with local public sector bodies. There should be a process of engagement between central and local government and industry to enable councils to fulfil their role to translate a national framework into transformative local plans that deliver on this agenda and invest in solutions for a green recovery and future.
3.3 Councillors and their councils have demonstrated local leadership throughout the pandemic and have shown that with the right tools and resources, councils can adapt and deliver at pace and scale for their communities and places. Councils have never been more trusted by their residents: polling conducted during June 2020 shows that 71 per cent of residents trust their council, an increase of 12 percentage points over just four months. Councils should therefore be trusted and empowered to deliver low carbon solutions to meet the net zero ambitions of Government and local communities.
Waste and recycling
Waste and recycling reform
3.4 Councils have kept waste and recycling services running during the COVID-19 outbreak, responding quickly to keep staff safe and deal with high volumes of household waste normally only seen at Christmas. In August, 52 per cent of councils reported that they were collecting up to 20 per cent more material for recycling from households than normal. Another three in 10 were collecting up to 50 per cent more recycling than normal.
3.5 Like many other services, waste and recycling has seen additional cost pressures and loss of income during the pandemic. A survey by the National Association of Waste Disposal Officers and partners in June 2020 showed the additional costs operating household waste and recycling centres. Additional monthly costs of at least £10,000 or more were incurred for almost three quarters of councils that responded in traffic management and almost one quarter in staffing.
3.6 The increase in tonnage of household waste and recycling was a notable and sustained impact of COVID-19 restrictions on movement, adding to cost pressures. Less visible, but highly disruptive to waste collection services was the increase in parked cars blocking access to roads. Cost has also been incurred through additional cleaning of vehicles and measures designed to allow collection crews to maintain a safe distance when working together, such as providing additional transport. Many councils have suffered a financial loss through the disruption of chargeable waste and recycling services, such as garden waste collection and commercial waste collection which was badly hit by the lockdown period. These costs must be fully funded through the Government’s work on managing COVID-19 pressures.
3.7 The COVID-19 outbreak has interrupted progress of the Government’s waste and recycling reforms, due to be implemented from 2023. Councils and the waste industry need clarity on the timetable for implementation and the detail of proposals. It is critical for councils to understand how the reforms to consistency, producer responsibility and the deposit return scheme for drinks containers will interact with each other and impact on the bottom line. A clear vision of implementation will give all stakeholders the confidence to enter into long term contracts and support investment in jobs and services.
3.8 For years councils have borne the cost for packaging recycling that should have been the responsibility of producers. We welcome the introduction of a new extended producer responsibility scheme that will require packaging producers and retailers to pay local authorities the full cost of recycling and disposal of their material from household waste. This funding should be paid in its entirety directly to councils and treated as additional.
3.9 We want to continue to work closely with Government on the detail of Extended Producer Responsibility and minimum service standards. For example, payments that are based on a notional ‘efficient’ service should not penalise councils for the reasonable challenges of delivering collection and disposal services in their individual local areas.
3.10 The Environment Bill will place new requirements on councils to collect a consistent set of materials for recycling including mandatory food waste collections. This must be fully funded through the new burdens process, including councils who are already collecting food waste on a voluntary basis. We support the principle of a core set of materials, but councils must be allowed to determine locally how waste is collected, taking into account the local geography and access to infrastructure for sorting and recycling.
3.11 Councils should continue to be able to charge for garden waste collection. Currently, around 65 per cent of councils apply a charge. Our engagement with councils indicates that residents are willing to pay for this service and there is little evidence of garden waste being diverted to residual waste as a result of the charge. Research for LGA and the District Councils’ Network found that extending garden waste collection to a comprehensive free service across England would add £175 million to costs, including disposal. At the same time the removal of charges would take £217 million out of council waste collection budgets, adding up to a total financial impact of nearly £400 million.
Waste and recycling infrastructure
3.12 The right investment in waste and recycling infrastructure will help towards the net zero target and the circular economy for resources. Councils have a strong track record in delivery, diverting millions of tonnes of household waste from landfill. In 2018/19 2.8 million tonnes of household waste was sent to landfill compared to 14 million tonnes in 2012/13.
3.13 We welcome the commitment to meet the new burdens arising from the implementation of the Resources and Waste Strategy. This must also include consideration of the impact on infrastructure and long-term contracts.
- Capital costs may arise in the implementation of the proposed core set of dry materials for household collections. The main gaps are on recycling of glass (collected by 80 per cent of councils) and pots, tubs and trays (collected by 77 per cent of councils). It should be possible for councils to add the remaining materials, although this may require changes to contracts and capital investment in new infrastructure such as vehicles and sorting technologies.
- Councils will need financial support to meet the practical and financial challenges of providing food waste collection services. This will vary by council, and there may be additional requirements for councils where there is no local infrastructure to process food waste. This will incur transport costs and may also require investment in additional capacity in waste transfer stations.
- Removing food waste and transferring more material from residual waste into recycling could impact on long term contracts for residual waste treatment. The transition costs will vary across councils, depending on local infrastructure and existing collection systems. This must be fully funded.
3.14 More broadly, further investment in the capacity of the UK’s recycling infrastructure is essential if Government wishes to expand the core set of materials collected from households and achieve its ambitions on increasing recycling rates for plastic, particularly low-grade plastics that do not currently have a ready market.
3.15 To help achieve reduction in landfill, councils are ready to play their part in consistent household collections, but this is only one part of the recycling system. The responsibility for stimulating markets for recyclate and delivering greater investor confidence is held broadly across a range of actors, and Government is ultimately responsible for the conditions in which the domestic market for reprocessing can be stimulated, including the delivery of necessary infrastructure.
Low carbon solutions
Unlocking local initiative
3.16 This Comprehensive Spending Review presents a unique opportunity for national government to empower locally-led action towards net zero carbon emissions. As councils and their partners plan for a green recovery from the pandemic and review their climate emergency strategies, Government can make great advances across areas such as skills and employment, including green jobs, decarbonising housing and transport, and inclusive economic growth, that supports Government’s commitment to levelling up the country. Councils are best-placed to take on this role and are already leading the way in delivering place-based low carbon solutions and projects.
3.17 Councils have expert localised knowledge of their places and residents and have been proactive in this area for some time. Our research of 100 councils’ activities found over 327 activities and projects related to tackling climate change. It also shows a diverse range of solutions by councils that capitalise on local assets, opportunities and partners to deliver meaningful and lasting change. Examples include the exploitation of geothermal potential in Cornwall through the United Downs Deep Geothermal project and, the UK Battery Industrialisation Centre in Coventry which harnesses the region’s leading position in the automotive sector.
3.18 If we are to meet the legal obligations established by the passing of the Climate Change Act (2019) and maintain the UK as a leading global example, Government needs to unlock councils’ full potential. Councils must have sustainable resources and funding flexibilities under local leadership to enable them to invest in place-based low carbon solutions for the long-term. For example, an LGA study of council activity to tackle the climate emergency indicates that councils need both capital and revenue funding. Capital investments ranged from £3,000 to install electric vehicle charging points, to £9 million with a completed solar farm in Cambridgeshire, to £28 million for a completed leisure centre combined with a heat and power plant at Eastleigh Borough Council.
Investing in renewables
3.19 To support the local implementation of low carbon solutions in every sector, industry and place, we need a resilient and flexible energy system that realises the full socio-economic benefits. Local authorities are significant consumers of electricity and by investing in green generation to meet their own needs, they can send a strong signal to businesses, residents and investors to help promote wider take up and investment in renewable energy sources, as well as providing a valuable income stream to support local services. As early adopters, local authorities can provide a pipeline of projects to stimulate growth in the low carbon energy sector.
3.20 The power sector has already been a major success story over the last 10 years, largely as a result of Government providing the right fiscal and policy support. For the first time in the UK’s history, renewables provided more electricity than fossil fuels at the end of 2019. As research commissioned by the LGA reiterates, increased global deployment of renewable energy technologies dramatically reduces their capital costs, which has enabled deployment to continue even as subsidies have fallen away.
3.21 A particular example of this is the onshore wind market, which has seen sustained growth since the late 1990s as the industry matured and the scale of turbines and size of developments increased, following government support. Nevertheless grid costs are a major consideration for new onshore wind developments and as the UK grid network becomes fully utilised, significant reinforcement is often required to allow new capacity to connect. Often, the cost needs to be covered by a project or cluster of projects connecting to the grid to achieve the economies of scale and make projects viable. While smaller projects can still be viable, levels of community support required also mean that very few schemes in England are likely to be deliverable. To deliver large scale projects, it may be necessary to consider the impact of the current planning system and whether that may need to change to enable low carbon energy infrastructure projects.
3.22 This is just one example of some of the opportunities and challenges of renewable energy facing councils. We now need to build on the success of the power sector and unlock its full potential as renewables take on a larger share of the UK’s energy supply. Councils can play a lead role in developing a flexible, low carbon, resilient energy supply if they are given the tools and powers. Realising the full benefits will require greater investment in and incentives for renewable energy solutions.
3.23 In particular, significant opportunities present in the green growth sector, if the approach to delivery is flexible and designed around place.
3.24 The full socio-economic benefits are far-reaching. For example, Imperial College outlines some of the outcomes for national security, where increasing the amount of renewable energy generated in the UK reduces our reliance on the import of fossil fuels from other countries and improves our energy security. At the international level, climate action reduces the chance of forced migration from climate-related disasters, which in turn may reduce pressure on immigration into the UK.
Developing the right skills
3.25 There is political consensus that the transition from fossil fuels to renewable energy will necessitate a shift in employment towards highly skilled jobs where the benefits are felt across all parts of the country. Councils can use their role as local leaders to bring together the skills and low carbon agendas to unlock growth in their areas, as shown in LGA commissioned analysis by Ecuity.
3.26 It found that nearly 700,000 jobs could be created in England’s low-carbon and renewable energy economy by 2030, rising to more than one million by 2050. Nearly half will be in clean electricity generation and providing low-carbon heat for homes and businesses (manufacturing wind turbines, installing solar panels and installing heat pumps). Around 40 per cent of jobs will be involved in installing energy efficiency products; providing low-carbon services, including financial, legal and IT; and producing alternative fuels, such as bioenergy and hydrogen. The remainder will be directly involved in manufacturing low-emission vehicles and the associated infrastructure.
3.27 Importantly, these jobs are projected to be generated across England’s local authorities and regions in the North, Midlands, East, South and London and, as demand for green jobs increases, it will require a diverse range of skills and local expertise to roll them out. For too long, employment and skills support has been centrally driven, meaning it often fails to meet and respond to local need.
3.28 An integrated and devolved approach to development of skills can achieve better outcomes for local communities and the economy. For example, a medium-sized combined authority could benefit from an additional 8,500 people each year leaving benefits and 5,700 people increasing their qualification levels, with additional local fiscal benefits of £280 million per year and £420 million to the economy. This could be delivered using the LGA’s Work Local proposal for devolving funding and powers over skills to local areas. It is explored in more detail in the Economy and Levelling Up chapter of this submission.
Housing decarbonisation
3.29 One of the most effective areas of focus when it comes to addressing carbon emissions is the built environment, with more energy-efficient homes reducing their reliance on fossil fuels.
3.30 The Spending Review offers an opportunity for additional capital investment for the delivery of environmentally friendly homes and commercial buildings. As a significant majority of the homes that will be in place by 2050 have already been built, this should include retro-fitting existing homes as well as new builds.
3.31 In particular, the Government should work with councils to urgently bring forward its commitment for a £3.8 billion capital Social Housing Decarbonisation Fund. This would provide a national stimulus to kick start the deep energy retrofit of all homes by investing in an energy revolution in social housing.
3.32 Analysis undertaken by Savills for the LGA estimates that the additional investment costs to achieve net zero carbon in existing housing stock held within councils’ Housing Revenue Accounts (HRA) is almost £1 billion per year over a 30-year pattern of investment.
Adapting to climate change
3.33 We have already begun to see the effects of climate change, not least over recent months, and it is clear that that the impact is not felt evenly across the UK. We have seen an increased risk of exposure to overheating and poor indoor air quality affecting the health of most vulnerable people; a dramatic rise in household water consumption where some areas such as the South West even lost supply; and greater demand for recreational services that have increased pressure on the natural environment.
3.34 Whilst the reality of the situation is significant, the future possibilities of climate mitigation and adaptation are far-reaching and there to be captured by the whole of the public and private sectors, if supported and mobilised by Government in the right way.
3.35 Benefits could be realised across not just the environment but health and the NHS, housing and inequality, employment, business and industry, infrastructure and security. Clearly, as these underpin many core services delivered by local government, councils have a significant role to play, whether by providing local leadership, adapting the services they deliver or working collaboratively with partners and others in their local areas.
- The Seasonal Health Intervention Network project of Islington Council and the Greater London Authority provides an example of how councils are approaching climate adaptation challenges that provide wider co-benefits. The project brings together health and housing practitioners to enable GPs of patients living in cold, damp homes to ‘prescribe’ double glazing, boilers and insulation to their patients in order to address the root-cause of their illness. The project reduces NHS costs as well as greenhouse gas emissions and improving the quality of the housing stock.
3.36 Despite the positive outcomes that this example shows, significant demands to reduce spending and rising demands for services, compounded by additional cost pressures following COVID-19, make it difficult for councils to have fully funded adaptation plans that ensure effective adaptation across all communities and service areas.
3.37 The ability of councils to be able to identify climate risks and have fully funded adaptation plans varies and depends on having the resources, capacity, skills, and partnerships. This requires both revenue and capital.
- For example, the overall budget for Birmingham’s Climate Change Adaptation Partnership work has been £370,000 over three years. Given the failure of existing tools to account for the fact that Birmingham’s city centre is already 4 degrees Celsius higher than the surrounding countryside, the partnership seeks to offer a range of tools and approaches to assess and identify which communities will need most help to adapt in order to effectively plan adaptation measures and priorities.
3.38 In a practical guide for local authorities, the Association of Directors of Environment, Economy, Planning and Transport (ADEPT) shows that investment in adaptation can be cheaper and more effective than the costs incurred responding to the impacts over the lifetime of the investment. This is supported by other evidence:
- According to the Environment Agency, for every £1 spent improving protection from flooding and coastal erosion, we avoid £5 of property damage. The multi-billion pound investment by Government announced this year to tackle flooding, which includes a plan to deliver flood and coastal defences, is expected to prevent £32 billion in economic damage.
- There is general international consensus on the economic benefits of adaptation, where the European Commission estimates that the cost to the European Union of not adapting to climate change would be at least €250 billion a year by 2050.
3.39 To put this into a local context, the examples of Glasgow and Leeds demonstrate the economic and wider benefits of investment in adaptation.
- The Climate Ready Cycle projects that climate change risks to the Glasgow City Region could cost £400 million a year by 2050 and, estimates an additional 5,700 extra heat-related morbidity cases and hospital admissions a year by 2050s, without adaptation measures. This is a significant cost not only economically, but to human life.
- Yet, there are substantial benefits to investing in adaptation, as demonstrated by the work of the Leeds Climate Commission. If Leeds were able to exploit the opportunities for energy efficiency and low carbon development, Leeds can save £348 a year for every person in the city by 2030 – that’s an annual total of £277 million – as well as create 4,200 extra years of employment. They show that simple, profitable improvements in heating, lighting, insulation and vehicles can reap significant results.
3.40 With the right tools and resources, councils can lead the way in creating resilient, net-zero communities and places. Long-term investment and funding is required to enable councils to bring partners together, have fully funded adaptation plans that can be implemented locally and realise the financial and societal benefits.
Flooding
3.41 Flooding can devastate communities, causing enormous disruption to families and businesses and resulting in huge clean-up bills. Investment in flood defence is vital in preparing for heavy rainfalls.
3.42 Councils are well placed to lead a local approach to flood defence, using their local knowledge to ensure that money is directed towards projects that best reflect local needs, including protecting key roads and bridges to keep local residents and businesses moving. Funding for flood defences needs to be devolved to local areas and sit within a new national framework for addressing the climate emergency.
3.43 In an emergency situation, the Bellwin scheme for emergency flood relief funding is vital for councils, but it often doesn’t cover the clean-up costs. Councils need to be able to access funding for these purposes, more easily and more quickly.
3.44 The new national flooding and coastal erosion strategy from the Department for Environment, Food & Rural Affairs (Defra) and the Environment Agency will need to be reflected locally in plans and strategies. This will require new skills and technical knowledge, such as natural flood management. We would like to work with Government on how councils will be supported to lead and implement the new strategy locally.
3.45 Lead local flood areas (LLFAs) were established in 2010 in county and unitary areas. Their roles include development of a local flood risk management strategy, investigating flood incidents and as statutory consultees, providing technical advice on surface water drainage to local planning authorities. Grant funding from Defra for LLFAs runs out at the end of this financial year and councils need urgent clarity on how this critical role will be funded from 2021.
Other environmental issues
Air quality
3.46 Councils are ambitious about developing and delivering local clean air plans.
3.47 To fulfil this shared ambition with Government, councils need to be sure that the costs of delivering these plans will be fully reimbursed through the implementation fund and that any additional costs because of unavoidable delays will continue to be met.
3.48 Councils also need assurances that the share of revenues from charging in clean air zones will allow them to cover the cost associated with administering the zones and will not be a long-term liability for councils.
Electric vehicles (EV)
3.49 In order to ease the transition to widespread EV adoption, the Government needs to reaffirm its commitment to support the current EV infrastructure charging grants and also to extend these schemes to benefit more places.
3.50 To drive value in infrastructure funding, the Government should consider a long-term approach which rationalises the number of funding streams available and provides longer term certainty of all capital infrastructure funding mentioned here and in other relevant sections of this submission. We believe this one-pot long-term approach could be extended to EV charging as well as other forms of infrastructure.
Nature and biodiversity
3.51 The Environment Bill will introduce new duties for public bodies to sustain nature and the environment, including a new system of biodiversity net gain in all new development.
3.52 We support this principle but have concerns about the implementation. In exceptional circumstances, where biodiversity measures cannot be delivered on site, the financial “credits” should be retained by local authorities so that funding stays in the area where development takes place. Local people can then have a say in how this funding can be used to improve the natural environment.
3.53 The assessment of new burdens will need to cover all the additional processes councils will be required to introduce through the nature and biodiversity measures in the Environment Bill, as well as ensuring that they have the right skills and training. For example, planning departments do not have the specialist ecological expertise to deliver the net gain proposals.
Trees and woodland
3.54 Trees and woodlands play a vital role in supporting biodiversity as well as providing valuable spaces for people to exercise and connect with nature. Supporting new trees and woodlands is a key part of national and local strategies for improving the natural environment and tackling the climate emergency. For example, Surrey County Council has put in place a strategy to facilitate the planting of 1.2 million trees by 2030.
3.55 However, our native trees such as ash and oak are under pressure from disease and climate change. Maintenance of trees in public spaces is vital to keep the public safe and slow the spread of disease to other parts of the country. Additional maintenance costs caused by diseases such as ash dieback and oak processionary moth are an additional finance pressure on councils.
3.56 The management of trees and woodlands needs to be part of the new national framework for addressing the climate emergency, that provides councils with enabling powers and funding to deliver effective responses.
3.57 Management of street trees should be a local issue. We do not support a change to legislation that would require councils to consult residents on the felling of street trees. If this policy is introduced, it must be treated as a new burden and councils must be fully funded.
Economy and ‘levelling up’
Homelessness
4.1 The pandemic has prompted a large-scale emergency response from councils’ homelessness services and their partners. A key driver of this has been the Government’s ‘Everyone In’ policy, which asked councils to ensure that people sleeping rough and in high-risk accommodation were safely accommodated to protect them, and the wider public, from the risks of COVID-19. The LGA supports this policy as a crucial element of the public health response to this crisis.
4.2 When the pandemic began, it was estimated that just under 4,300 people were sleeping rough. Since March, MHCLG figures suggest that councils have accommodated 15,000 people under Everyone In, in addition to working with a wide range of local partners to coordinate support for people brought into emergency accommodation, many of whom are experiencing the multiple needs associated with rough sleeping.
4.3 This work has performed a vital role in reducing the risks of COVID-19 to people experiencing homelessness, whom evidence suggests are particularly medically vulnerable to the effects of the illness. There is also increasing evidence of the wider impact that this response has had on the broader wellbeing and health outcomes of people in emergency accommodation.
4.4 However, the work has also created a significant strain on councils’ resources, adding to existing financial pressures. MHCLG data on councils’ finances from July 2020 indicates that councils forecast an additional expenditure of £99 million on homelessness services, and £144.6 million on rough sleeping, as a result of COVID-19 in 2020/21.
Links between housing policy and rises in homelessness
4.5 The Government’s housing policy in recent years has focused on support to the private sector to increase the delivery of new homes for home ownership. The 2019 UK Housing Review found that, between 2018/19 and 2021/22, government investment in affordable housing will account for only 26 per cent of the total.
4.6 Within that, the most recent data from the government’s Shared Ownership and Affordable Homes Programme 2016-2021 showed that only 4 per cent of the funding up to September 2019 has been allocated to the delivery of social rented homes.
4.7 Subsequently, long-term declines in social housing and home ownership have led to the rapid growth of the private rented sector (PRS), which has doubled in size since 2002 to comprise 19 per cent of all households in England in 2018/19.
4.8 Evidence from the National Audit Office suggests that the decreasing affordability of private rented housing has been one of the key factors behind increasing PRS evictions, which in turn has been one of the key drivers in recent years behind increases in statutory homelessness. Across England, the ending of private rented sector tenancies accounted for 74 per cent of the growth in households qualifying for temporary accommodation between 2009/10 to 2016/17.
4.9 Another key factor has been caps on local housing allowance (LHA) rates, which have reduced households’ ability to cover the costs of housing in the private rented sector. LGA analysis has found that, for every 1,000 households experiencing a rent shortfall as a result of LHA caps, 44 require temporary accommodation, creating average gross accommodation costs over between £1.4 million to £3 million for every council with homelessness responsibilities.
4.10 Councils’ gross spend on temporary accommodation was £1.1 billion in 2018/19 and recent LGA analysis found that councils’ net expenditure on temporary accommodation was over budget by £140 million per year in 2018/19. This is a statutory service, and overall spend on accommodating homeless households has increased 372 per cent between 2009/10 and 2018/19.
4.11 Almost all councils are currently delivering homelessness services well beyond the statutory requirements of the Homelessness Reduction Act, despite the funding challenges involved. A survey carried out by the LGA in 2018 found that 29 per cent of responding councils did not think they had been sufficiently resourced to deliver their new duties, even in terms of the additional burdens and processing requirements of the Act.
4.12 Moreover, the continued rise in the number of households in temporary accommodation undermines the assumption in the new burdens assessment of the Act that the costs to local authorities of providing temporary accommodation would be neutralised by year two of the Act’s implementation. The situation is particularly acute in London, where, as highlighted by recent London Councils research, costs for elements such as temporary accommodation are higher than in other parts of the country.
4.13 As a result, councils are seeing increased proportions of funding being diverted towards temporary accommodation, which reduces their ability to provide the preventative services which would have eventually driven down costs. As detailed by the National Audit Office, local authority funding pressures threaten the continued provision of these non-statutory services, and expenditure on housing services (excluding housing benefits) saw a reduction of £1.3 billion in real terms between 2009/10 and 2018/19.
The case for shifting to homelessness prevention
4.14 Recent academic analysis suggests that the primary focus of government funding in recent years has been the management of new homelessness, and particularly rough sleeping, with the Rough Sleeping Strategy, published in 2018, introducing several additional funding streams to support the Government’s commitment to ending rough sleeping within this parliament.
4.15 The Homelessness Reduction Act 2017 also introduced new statutory responsibilities on councils, including a reinforced prevention duty extended to households without priority need.
4.16 However, governments’ homelessness policy has not yet focused on the key drivers of homelessness, including a lack of affordable housing, welfare-related poverty, and a lack of an integrated prevention approach.
4.17 As a result, councils continue to see high numbers of households presenting as homeless and accommodated in temporary accommodation. Statutory homelessness statistics show that on 31 March 2020, there were 93,000 households in temporary accommodation – a 9.4 per cent increase on 31 March 2019.
4.18 The economic impact of COVID-19 has created a risk of much greater homelessness pressures as a result of poverty. Recent UK labour market statistics show that the economic impact of the pandemic has resulted in at least 730,000 fewer people in work since March.
4.19 The added pressure for low-income households, set against the context of existing need, creates an impetus to stem the flow of all forms of homelessness. The key policy objectives must be to:
- ensure effective rehousing and support for the 15,000 people who have been accommodated in emergency accommodation
- improve the preventative response for households at risk of homelessness, including those at risk of street homelessness, to enable them to sustain their housing
- ensure the move-on of households in temporary accommodation into settled housing.
4.20 This requires a funding and policy settlement that addresses affordable housing, welfare and labour-related poverty, and integrated prevention. Our recommendations relating to affordable housing and welfare reform have been addressed elsewhere in this submission.
4.21 We are seeking an explicit, national-level focus on homelessness prevention work, and an associated funding regime, that enables and encourages councils to avoid residents reaching crisis and reduces the demand for emergency responses.
4.22 This must recognise that homelessness prevention is not something that councils – who hold statutory homelessness prevention responsibilities – can do alone, but requires a combination of action from national government, local government, and their partners in the public, VCS, and private sectors. It must also encompass a wider focus on who can be usefully reached and targeted by preventative services, such that prevention becomes about people facing unexpected income shocks, struggling to pay the rent or other household bills, or approaching a stressful transition point in their lives.
4.23 In upcoming research, the LGA has used a definition of homelessness prevention based on the St Basils Positive Prevention Framework, and subsequently used in the West Midlands Homelessness Taskforce plan to design out homelessness in the region.
Reforming homelessness funding
4.24 Currently, funding for homelessness services does not enable councils to meet this ambition. New funding, whilst welcome, is fragmented, with recent LGA analysis showing that 12 small, short-term funding programmes relating to homelessness were issued between 2015/16 and 2018/19. In most cases, these programmes are specifically focused on the emergency response to existing rough sleeping.
4.25 Moreover, funding is often issued on a short-term basis, creating negative impacts on staff retention, long-term strategic planning, and joint commissioning. Councils are also increasingly asked to bid for this funding through a competitive process, with half of the new homelessness grants allocated in this way. This is placing extra stress on an over-stretched homelessness system, as officers are often required to scope and complete an extensive application within limited timeframes – sometimes as short as one month.
The £266 million Next Steps Accommodation Programme (NSAP) was launched by MHCLG on 18 July 2020, with the aim of making resources available to councils to help ensure that 15,000 people continue to have a safe place to stay. The LGA welcomed this funding and shares its aims.
However, councils have raised the following issues relating to the programme:
Competition – following the request to councils to accommodate all rough sleepers on 26 March, councils have acted in good faith to meet this significantly increased demand and have accommodated 15,000 people in emergency accommodation. The competed nature of the funding programme means that only a selected number of councils will recoup their costs from this work. It has also required them to engage in an intensive bidding process, diverting resources away from service delivery at a time of intense pressure.
Short timescales – councils have been asked to provide match funding for any capital funds received through the programme, and do not feel that this expectation is deliverable within the timescales: given funding pressures, it has proven difficult to identify existing capital funds which can be re-allocated, and councils have been told that they cannot use Right to Buy receipts towards this programme. The March 2020/21 deadline is also very short for delivery of new capital schemes, particularly with the 10 per cent limit on the amount of funding which can be used to convert or re-utilise existing social housing units.
Uncertainty – funding is focused on specialist supported housing with a maximum limit on tenancies of only three years, secure tenancies excluded, and revenue funding only available for four years. However, councils must also commit to maintaining any supported housing units created for 30 years – this requires them to make long-term investment decisions based on short-term funding. It would also lock councils into diverting resources into a stock of short-term housing with short-term support, rather than the stable, long-term support that they feel is needed to support people with complex needs out of homelessness.
Restrictions on support provided – councils are ambitious in their plans to support rough sleepers and feel that the restrictions in the guidance prevent them from delivering the long-term, flexible support needed. In particular, the implication that support is tied to the tenancy rather than the individual excludes Housing First schemes from funding, as well as any approaches where individuals are supported by the same worker and specialist agencies throughout the housing pathway. Requiring councils to attach different support to different interventions is less efficient, and also risks poorer outcomes for individuals
4.26 Our research on homelessness prevention found that councils seek a set of funding arrangements that allow them to both plan and invest in homelessness prevention and minimise the need for emergency responses. In particular:
- Funding should be adequate, addressing the large funding gap in local authority homelessness services. There must also be adequate funding for all homelessness related local services, including mental health, adult and children’s social care, and drug and alcohol services, so that these services have the capacity to better engage with homelessness prevention partnership working arrangements and households at risk of homelessness.
- Funding should be joined up and flexible, with local homelessness strategies acting as the main vehicle through which homelessness funding is delivered, and homelessness prevention is collectively organised, owned and delivered.
- Ideally, it should be delivered as a single, flexible fund via councils which is usable across public services towards a shared definition of ‘homelessness prevented’, supported by joined-up funding across central government departments for local agencies. This would reflect the fact that a service being scaled back has repercussions across the whole public purse and would allow for more flexible and appropriate commissioning.
Working across government to prevent homelessness
4.27 As part of the drive towards improved homelessness prevention, we are seeking a joint statement enshrining a national commitment from every government department to preventing homelessness. This should explicitly acknowledge departmental responsibilities in delivering the Homelessness Reduction Act, and include a set of departmental actions to take, such as joint approaches to information, protocols, partnership, case management, training, monitoring, reviews, and commissioning to maximise the value from collective investments.
4.28 It should address funding for all homelessness-relevant local services to enable access to timely support, with a commitment to integrated social, health, drug and alcohol, and economic support through transition points between key services and beyond.
4.29 This would be underpinned by the extension of the Homelessness Reduction Act ‘duty to refer’ to a ‘duty to cooperate’ on relevant public agencies, with each department determining a definition of ‘homelessness prevention’ and key success factors, and developing clear and detailed guidance and training for all service managers, commissioners and staff in delivering the action plan through effective multi-agency working locally.
4.30 This joined-up approach also needs to be underpinned by improvements in homelessness data, to be determined in close collaboration with councils and their partners to monitor the impact of departmental actions on a shared definition of ‘homelessness prevented’ and secure the buy-in of local agencies in tackling homelessness locally:
- Any homelessness data currently collected from councils, and particularly the data from the Homelessness Case-Level Collection (H-CLIC), should be made more visible and accessible for councils’ own use.
- Councils should be supported to capture data on individuals who present before the 56-day homelessness prevention duty period. This should include measures to improve data linking between services, so that councils are able to understand the impact of other agencies’ actions and identify households at early risk of homelessness.
- Guidance on GDPR to departmental agencies should be improved, to overcome existing barriers in data linking.
Addressing housing insecurity
4.31 The Government should urgently bring forwards its proposal to end Section 21 evictions. Doing this would address one of the key drivers of homelessness since 2010, and therefore reduce demand for temporary accommodation and stem the increases in costs set out above.
4.32 Steps should also be taken to enable councils to enforce against illegal evictions:
- Ensure sufficient funding for council tenancy relations officers (TROs): TROs support tenants in cases of illegal eviction. They operate in parallel with environmental health officers. However, they do not have parallel powers to investigate illegal evictions, and – like EHOs – have been severely affected by cuts to local government funding which should be addressed.
- Ensure greater flexibility for landlord licensing schemes: Landlord licensing schemes can have significant benefits in respect of enforcement of standards in private rented sector accommodation, including illegal evictions. However, local authorities lack the flexibility to take forward whole area or area-specific licensing schemes. From April 2015, councils have been required to secure Secretary of State approval for licensing schemes that cover more than 20 per cent of the area or 20 per cent of privately rented homes. This threshold should be removed to enable councils to take greater action against illegal evictions and reduce emergency homelessness.
4.33 The Government should also address the drivers of rising evictions and homelessness, by addressing the unaffordability of housing. Our recommendations on welfare reform and affordable housing have been addressed elsewhere in this document. In addition to these, the Government should universally and temporarily lift the No Recourse to Public Funds condition, so that all migrants have access to welfare and employment support and can avoid poverty and subsequent homelessness. Supporting individuals with No Recourse to Public Funds continues to be a significant unfunded burden for local authorities. In 2018/19, 59 councils were spending £47.5 million per year on NRPF service provision. This is particularly vital in the context of the pandemic, to enable all migrants to access welfare provision, avoid poverty and subsequent homelessness, and self-isolate in the event of future local outbreaks.
Costs to councils of asylum dispersal
4.34 Councils and government are working together to achieve a more equitable and place-based approach to the accommodation and support of dispersed asylum seekers in order to reduce disproportionate impacts in certain regions and councils.
4.35 In July 2019, the Government and councils agreed a ten-year plan for the proportion of supported asylum seekers housed in each government region and devolved administration to reflect each region’s share of the UK population. As of March 2020, 180 of 382 (47 per cent) of local authorities have agreed to have asylum seekers dispersed in their area. This figure only includes principal local authorities with housing responsibilities and therefore does not include English county councils.
4.36 Councils raised the lack of funding for their role in the dispersal system as a significant barrier to future participation in any current or revised scheme.
4.37 Asylum dispersal has a cost impact as a result of local governments’ statutory obligations, particularly on homelessness, education and children’s and adult social care, all of which have ongoing resource challenges detailed above. As well as the additional costs of meeting statutory responsibilities in supporting vulnerable groups and meeting the specific needs of the cohort, there is also additional staff time involved in working with providers on the procurement of accommodation and costs associated with other council responsibilities, such as maintaining community cohesion.
4.38 At the end of March 2020, latest government statistics indicate that 44,244 asylum seekers in the UK were in receipt of support under Section 95 of the Immigration and Asylum Act 1999, with the majority (83 per cent) located in England. An additional 4,077 individuals were in receipt of support under Section 4 of the Immigration and Asylum Act 1999 which provides refused asylum seekers without children with housing while they take steps to leave. 2,577 were in receipt of support under Section 98 which provided for asylum seekers on a short-term basis while their application for Section 95 support is considered.
4.39 There is no dedicated funding available to fund councils’ role in the dispersal system. Ad hoc funding streams have been made available to some councils through a bidding process in England via the Controlling Migration Fund or limited funding from the European wide Asylum, Migration and Integration Fund (AMIF). On the basis of information from several councils, all with asylum populations of over 650 and all of whom had been asylum dispersal areas for at least five years, the average unfunded cost per service user per year was an average of just under £2,500.
4.40 These figures include potential costs to councils of supporting those at the end of the asylum decision making process who have No Recourse to Public Funds (NRPF). Statutory support that councils may need to provide for destitute families is not currently funded. An annual report from the NRPF Network showed 66 local authorities supported 2,450 households at an annual cost of £44 million at year end.
4.41 It is clear from the data returns that there is identifiable expenditure in relation to being an asylum dispersal area, though further work beyond this initial scoping exercise to capture costs may be required. In order to enable other local authority areas to participate, there have to be relevant services in place to support asylum seekers and the local community and this scoping exercise did not consider positive models of community support and what funding is required by councils to the community and voluntary sector for these.
4.42 We are calling for per capita grant funding to meet councils’ costs, reflecting the current funding for refugee resettlement and support for UASC (the latter is covered in more detail in the care and health inequalities chapter). We would like to continue to work with government to develop a system based on partnership work, shared oversight and transparency, with a reduction in hotel use and destitution.
4.43 The Home Office designed the five-year funding model for refugee resettlement schemes jointly with local government in 2015 and this partnership model could be used when addressing the cost pressures in dispersal.
4.44 Councils are eager to build on their strong track record of supporting those resettling in new communities and are pleased the Government confirmed it will continue the resettlement scheme after 2020. Key to the success of this programme had been long term funding which allowed councils and partners to effectively plan for new arrivals and their integration into new communities. It had been confirmed that councils will receive initial one-year funding to deliver the scheme. Funding for future years at the same level needs to be followed through in the Comprehensive Spending Review.
4.45 We remain keen to work with government so that clear links are made across all the programmes that resettle any new arrivals. A new immigration route for British National (Overseas) citizens wishing to leave Hong Kong may have cost impacts for councils, both in terms of the impacts on local services of large numbers of rapid arrivals and also supporting those without access to public funds who may become destitute. Councils are keen to receive any further planning assumptions on the potential numbers of arrivals and involvement in any new burdens assessment. Any resource impacts on councils of the EU Settlement Scheme, particularly on the support provided by children and adults services and for those who may not complete the process by the June 2021 deadline, should also be fully funded.
Digital connectivity
4.46 The Government has committed to delivering gigabit-capable broadband to all premises by 2025 and, earlier this year, signed an agreement with mobile network operators to improve mobile coverage across rural areas via a Shared Rural Network by 2026.
4.47 Councils fully support these ambitions and, over the last decade, have played a vital role coordinating the public roll out of superfast broadband and catalysing the wider commercial expansion of digital infrastructure. They have also been key to barrier-busting local issues including:
- challenging, sense checking and optimising publicly funded interventions and broadband deployment plans using local knowledge of communities, politicians and geographies to help mitigate delays, cost escalations and local complaints
- leveraging opportunities to accelerate deployments, reduce costs and stop unintentional overbuild
- helping secure complex wayleaves agreements with landowners to use their land to host digital infrastructure
- enabling streetworks access to 166,000 miles of local roads whilst protecting the structural integrity of the network, via inspections of works.
4.48 It is estimated that the total public and private investment committed to rolling out gigabit-capable broadband will reach £30 billion by 2025. This includes the £5 billion pounds committed by Government to subsidise roll out to the final 20 per cent of area and is the largest investment in the country’s digital infrastructure network to date.
4.49 However, an infrastructure programme of this scale requiring a substantial amount of streetworks, land access negotiations, community engagement and other local deployment activity, will inevitably face a range of roll out challenges and potential delays.
4.50 This could have significant consequences for the country and the Government’s 2025 deadline. Recent analysis has also shown that even a 12-month delay to achieving the Government’s full coverage of gigabit-broadband ambitions could cost the UK £9.7 billion of productivity benefits.
4.51 The Comprehensive Spending Review presents a golden opportunity to empower councils to help the Government’s ambitions become a reality across local areas. To do this, Government must provide funding for councils to put in place a local digital champion to help coordinate delivery locally and to recruit extra capacity within highways and planning teams to respond to surges in local roll out activity, such as streetworks permit requests or planning applications, that take place when a provider commences roll out in a specific area. This will be essential to avoiding local bottlenecks and the slowing down of delivery. A local digital champion would be a central contact point for government and broadband providers to help problem solve deployment issues in the local area.
4.52 Councils cannot create these positions without financial support. With the effects of the pandemic, many are under even greater financial pressure and will be unable to prioritise vital barrier-busting work over key statutory services. This could place a significant risk on the Government’s delivery timescales.
4.53 Analysis undertaken by ADEPT’s Digital Connectivity Working Group has recommended that councils have access to £200,000 of flexible grant revenue funding from Government annually until 2025 in order to fund this capacity. This would represent an annual commitment by Government of £30 million and would equate to less than 3 per cent of the £5 billion it has already committed to rolling out gigabit connectivity.
Skills and employment
4.54 With millions already displaced from the labour market and needing to find work and reskill due to the COVID-19 crisis, it is essential we align job creation and employability measures, so no community is left behind.
4.55 To make this happen, we need a co-designed, locally integrated and delivered employment and skills offer within a broad, flexible national policy and funding framework, which should enable local and national leadership to combine efforts to plan a recovery that works for all areas. This should include:
- A COBRA-style response for jobs and skills to maintain political focus, urgency of action and dialogue, bringing together government, local and combined authorities, sector and trade representatives and key stakeholders.
- Local jobs and skills taskforces coordinating a local plan using existing structures which recognises the different needs and delivery routes within places, bringing relevant partners together to pool local expertise and coordinate resources building on ‘rapid response’ models to support a green economic recovery.
- A multi-year, flexible, outcome driven local funding pot combining careers advice, back to work, training support (increased adult education budget (AEB), plus National Skills Fund and National Retraining Scheme), some apprenticeship funding and EU funds/UK Shared Prosperity Fund (with additional national resources as required), enabling local partners to make swift decisions for their local businesses and residents.
4.56 The approach to apprenticeship funding needs radical change. If the Government increased Apprenticeship Levy flexibilities, including allowing public pooling of funds, pausing its expiry policy, and devolving non-levy funding, councils could support the local economy by bringing much needed coherence to the system locally. It would allow them to target sectors, address local supply- and demand-side issues, widen participation to disadvantaged groups and specific cohorts, with a proportion spent on pre-apprenticeship training and administration of programmes.
4.57 With the risk of further lockdowns hindering employer confidence, establishing and scaling up local ‘training agency’ models could help businesses’ recruitment needs and move more people into work.
4.58 Alongside these measures, we are also calling for a levy payment holiday (up to six months) for businesses struggling with cashflow problems and allow employers to collaborate on transferring/pooling.
4.59 Furlough has masked the real impact of the crisis, but with the scheme due to end in October with no nuanced sector, geographic, or employer size plans in place, we can expect high volumes of clustered redundancy in local areas, and we would welcome discussions with government about what further steps can be taken for sectors and/or areas hard hit.
4.60 Young people need a clear local offer that brings together the welcome government investment into new and existing support for young people including Kickstart, the Youth Offer, sector-based work academies, apprenticeships, T levels and traineeships. This can only be brought together by local government using its economic development and statutory duties.
4.61 To enable this to happen, the Government must provide councils and combined authorities with additional powers and specific resources to coordinate provision and commission supplementary programmes to plug any identified gaps locally. This will help support economic recovery and better support those who are NEET, or those at risk of becoming NEET, to make an effective post-16 transition. We are in a prime position to make a success of Kickstart, as large employers and by supporting other local employers to take up these opportunities if they have the funding to lead local coalitions or intermediaries, or directly deliver as accountable bodies.
4.62 We need to work together to support adults to find work or reskill. The Government should work with us to co-design a plan to support the long term unemployed and increase and re-purpose skills investment to retrain people into local in-demand jobs (green jobs, social care, etc).
4.63 People need flexible, training courses with maintenance grants delivered through a local provider base funded by at least doubling and fully devolving the AEB to £3 billion, bringing forward National Skills Fund and National Retraining Scheme budgets, and publicly funding Level 3 qualifications by turning the adult learner loans into a skills budget.
4.64 Moving beyond recovery and thinking ahead to the Devolution and Local Recovery White Paper, this is a unique opportunity to ‘Re-think local’. The Government should back and fund the trialling of the LGA’s Work Local model, an integrated and devolved employment and skills system.
4.65 This is a blueprint for skills and employment devolution that works for all people and place which could, for a medium sized combined authority, lead to additional fiscal benefits for a local area of £280 million per year, with a benefit to the economy of £420 million. This would be associated with an additional 8,500 people leaving benefits, an additional 3,600 people achieving Level 2 skills, and an additional 2,100 people achieving Level 3.
4.66 Government should also ensure that funding streams for delivering skills training and development are accessible to cultural organisations that are currently unable to operate viable models under social distancing. These organisations will not only be able to contribute soft skills training that contributes to levelling up a community, but also offer large facilities that lend themselves to socially distanced face-to-face training sessions.
4.67 Working with universities, councils and other education providers, these facilities can be brought in to provide key skills training while also supporting our cultural infrastructure to survive through to the point where they will again be independently financially viable.
The welfare system and local safety net
4.68 Councils continue to provide significant support to low income and disadvantaged households. This support complements the Government’s wider programme of welfare reform to prevent hardship and build resilience.
4.69 The response to the pandemic quickly demonstrated that councils were best placed to understand the specific impacts in their local area, and to work with partners to provide quick, effective and integrated help to those facing financial hardship or economic vulnerability.
4.70 In response to COVID-19, the Government put in place some short-term financial measures to enable councils to provide support to those struggling to afford food and other essentials. In many places this was able to map on to existing local schemes, which had been sustained by councils, alongside the mainstream welfare system.
4.71 Councils have found it increasingly difficult to maintain local welfare provision since the removal of separately identified funding in 2015. A wide coalition of VCS partners recently highlighted the vital importance of restoring local welfare funding to councils to sustain support for vulnerable people in the wake of the pandemic. Those partners made the case for £250 million of identified funding to go to English councils.
4.72 When aspects of the social fund were devolved to councils from the DWP in 2013/14, funding was £176 million per annum. The Comprehensive Spending Review presents an ideal opportunity to fully restore core, separately identified funding for local welfare schemes set at this level as a minimum, to ensure that all communities are fairly and effectively supported throughout recovery and beyond.
4.73 The most recent analysis of debt advice provision by the Money and Pensions Service (MaPS) identified that nine million UK adults are ‘over-indebted’ and demand for debt advice far exceeded supply, with around 40 per cent of demand being met.
4.74 Since that research was published in June 2019, MaPS have been working hard to expand provision through a range of initiatives such as the PACE pilot, and to improve referral pathways. Councils are a key partner – as creditors, as commissioners and providers of advice, and as a source of referrals. The impact of the pandemic presents real and substantial risks around problem debt. The Spending Review needs to ensure that councils have the resources to sustain crucial partnership working with MaPS and advice providers.
4.75 Government is placing an increasing emphasis on preventing problem debt and promoting financial inclusion. With the right funding and flexibilities councils could accelerate work with credit unions, community development finance institutions (CDFIs), advice providers and financial services providers, to engage with households through their existing financial relationship with the council, for example via council tax or rental liabilities, to improve inclusion and capability.
4.76 The Comprehensive Spending Review is an opportunity for Government to continue to invest in improved fairness and efficiency in local debt recovery by enabling councils to invest further in data-sharing and preventative support. This could include expanding the successful pilot between HM Revenue and Customs, Cabinet Office and councils.
4.77 Research by Citizens Advice identified the harm and inefficiency that arises from lack of flexibility in council tax regulations that make it hard for councils to initiate a deduction from benefits without getting a liability order. Councils identified an increase of £500 million in council tax arrears between March and June, making it more important than ever for councils to be able strike the best possible balance between supporting vulnerable customers and recovering vital income. We would like to work with Government to urgently review council tax guidance and regulations to ensure that councils are able to identify and support vulnerable households, whilst also ensuring that all those who are able to, meet their liabilities.
4.78 Support for households facing economic vulnerability will be crucial to ensuring the success of wider measures to address health inequalities, homelessness, digital and social exclusion and a changing employment market.
4.79 The LGA has worked closely with government and councils throughout the implementation of Universal Credit and wider welfare reform. 2.9 million new claim applications for Universal Credit were made between 16 March and 9 July 2020. This placed considerable pressure on the DWP, who rightly focused on ensuring claims were processed and put into payment as efficiently as possible.
4.80 Councils have continued to provide support to households as they adapt to reforms and changes in household income. Councils must now receive the support, information and funding from Government they need to support and advise those now managing on a lower income, particularly those with other vulnerabilities, both efficiently and effectively.
4.81 The Comprehensive Spending Review provides an opportunity to strengthen partnership working, provide sufficient resources and greater clarity about the long-term relationship between councils and the DWP to ensure that households receive effective, integrated advice and support. This will be crucial to fair and effective social and economic recovery.
4.82 Research commissioned by the LGA shows that restoring the LHA rate to the 30th percentile of market rents could save councils with homelessness responsibilities an
average gross cost of providing temporary accommodation of between £1.4 million and £3 million. It is vital that the Government uses the Spending Review as an opportunity to maintain the LHA rate at least at the 30th percentile of market rents.
4.83 Discretionary Housing Payment (DHP) enables councils to provide vital support to households facing a temporary shortfall. However, DHPs have increasingly been used as a panacea for shortfalls that result from welfare changes and housing policy.
4.84 The DWP is monitoring council spending on DHP during the pandemic. However, councils have highlighted that demand for DHPs will currently be suppressed by measures such as the ban on evictions. Shelter estimate that the number of private renters in arrears doubled over the summer to around 227,000. Research conducted by HouseMark showed that social sector arrears were £100 million higher in May 2020 than at this stage in previous years.
4.85 This alone suggests that as other COVID-19 support expires, councils are likely to face a significant increase in demand for DHPs. Councils are currently prohibited from carrying over DHP funding between financial years and face a lack of certainty about future funding. It is vital that the Comprehensive Spending Review ensures that funding for DHP and other local discretionary support is both adequate and fit for purpose.
Roads and public transport
Roads and transport infrastructure funding
4.86 There is much more that councils would like to do to improve their local transport networks, but they are hampered by the relatively low resource base as a result of previous reductions in funding.
4.87 For example, NAO figures show that local authorities’ overall non-social care spend went down by 33 per cent in real terms between 2010/11 and 2016/17, with highways and transport services, including highways maintenance, experiencing a 37 per cent cut. This has impacted on their ability to deal with day-to-day issues such as tackling potholes, dealing with streetlighting issues, as well as their ability to respond to the decarbonisation agenda, such as supporting active travel, or dealing with poor air quality.
4.88 Road and infrastructure projects involve a wide range of funding procedures across tiers and agencies, including variations in how funding is announced, recorded, published and monitored. The fragmentation in local government funding undermines central government’s understanding of service delivery as a whole and of the interactions between service areas.
4.89 When combined with conflicting objectives, priorities, funding mechanisms, geographies, and accountability regimes in other services, fragmented local government funding risks driving different parts of the public sector apart rather than bringing them together.
4.90 The increasingly frequent project-basis for determining and allocating grants has undermined the ability of councils to plan strategically for the long term. It limits time for commissioning and risks harming the quality and value for money of the projects we plan. As a result, staff may be hired on short-term contracts, strategies may be reduced in scope, and joint commissioning is also limited, as councils are unable to guarantee certainty to partners.
4.91 Councils are too often asked to bid for funding through a competitive process. In many cases, this has led to resources being diverted towards the application process, placing additional stress on an over-stretched system. In many cases, the timescales for application are limited.
4.92 Excessive reliance by government on short-term competition funding for the long-term task of transforming transport networks is inefficient and costly. For example, the Urban Transport Group has concluded:
- the costs of competition funding are high – for example, the cost of bidding for the Transforming Cities Fund was in the region of £1 million for one combined authority
- the costs of preparing a bid for a small scheme is disproportionately high when compared with a large scheme – for example, the cost of bidding for a £5 million project is typically two to five times less than bidding for a £100 million project, despite the reward of the latter being twenty times greater
- bidding for short-term projects is a major drain on limited available staff, whose time could be better used for urban transport planning and delivery.
4.93 Even using conservative assumptions, they found that:
- the typical cost of bidding for a £5 million project ranges from £35,000 to £94,000
- the typical cost of bidding for a £100 million project ranges from £170,000 to £339,000.
4.94 In addition to the problems we have identified in bidding for these grants, assessment processes often favour car journey times and underweight the wider benefits of other modes of transport.
4.95 We have long supported the idea that capital expenditure should be funded through long-term secure grants to councils in order to plan a holistic pipeline of infrastructure and capacity improvements focused on the needs of local networks as a whole.
4.96 In particular, we support the proposals in the National Infrastructure Assessment of guaranteed five-year spending pots for this purpose. This would mean long-term investment in public transport infrastructure could be supported by councils.
4.97 In addition:
- The Government should fully commit the £3 billion outstanding funding announced in February for bus improvements to be allocated as soon as possible.
- Councils need additional funding to address the £11 billion backlog of repairs and reduce the need to undertake more expensive pothole repairs. Clearing the backlog prevents the need for more costly and disruptive renewals works later.
Buses and public transport
4.98 Coronavirus restrictions and the need for social distancing on buses destroyed the commercial funding model for bus services. At present, bus services are completely dependent on emergency government funding support, much of which is paid through councils.
4.99 It is likely to be some time before a commercial model for operating bus services can return. However, the emergency has also shown that essential workers need the bus to get to work and places cannot function without a bus service. Getting by without a bus service is simply not an option.
4.100 The bus also needs to play a bigger role in the future if we are to make rapid progress towards decarbonisation. This will require a concerted effort to rebuild confidence in bus services in the medium term and to address the shortcomings of service provision.
4.101 Whilst different forms of public-private management of the bus system could emerge after coronavirus, the critical issue is whether the right conditions will be created for the bus. This means addressing every aspect of the journey from access to bus stops to the quality of the vehicles. Councils will have to provide road space for bus priority to deliver faster journey times. It also means ensuring that pricing for cars and buses makes bus use the more attractive option.
4.102 However this is managed, it requires more support for the bus than has been delivered in the past two decades.
4.103 Councils are currently making concessionary payments on the basis of pre-COVID-19 travel levels. This means the link between concessionary payments and the number of journeys is effectively broken. Local authorities were requested to do this by the Department for Transport (DfT) as an emergency measure and we are increasingly concerned about its sustainability and legality.
4.104 Concessionary fares were underfunded by approximately £700 million per year before the crisis. This meant that local funds were being used to prop up a national scheme. With the onset of COVID-19 and the direction to break the link between payments and actual journeys, we are now in a position where large amounts of local taxes and revenues are being used to directly sustain private businesses. The shortfall should be permanently addressed through the Comprehensive Spending Review.
4.105 Home-to-school contracts are an important source of revenue for the bus and coach sector and give them long-term and predictable revenue. They act as a means of maintaining capacity in the sector.
4.106 As an emergency measure, councils had been asked by the DfT to continue to pay for home-to-school contracts at the full pre-COVID rate. Given that most children have stayed at home, during the national lockdown stage of the pandemic and many schools were closed, councils continued to pay for spare capacity. This meant that money intended for council home-to-school transport budgets was diverted towards sustaining commercial bus and coach operators.
4.107 We cannot continue to rely on a centralised model of DfT subsidy for a network that bears little or no resemblance to the realities of the recovery period.
4.108 This unprecedented situation presents an opportunity to develop a new and targeted method of defining and paying for a core public transport network that we, as a country, are prepared to support regardless of its viability. That is the network we should be prepared to support regardless of the progress of the pandemic and should rely on public subsidy if necessary.
4.109 Defining and commissioning that network is a job best suited to councils. They have the local knowledge of transport networks and community needs in order to make informed decisions. They also have local legitimacy to distribute payments to ensure the network is sustained.
4.110 An initial step towards this ambition could be the devolution of Bus Services Operators’ Grant payments to councils. We have long argued that the current system of subsidising fuel does not target money effectively and works directly against our clean air goals. Devolving the money to councils to support socially useful services would be a more effective measure.
UK Shared Prosperity Fund
4.111 The UKSPF is a significant opportunity to promote local growth and reduce regional disparities and drive economic recovery. However, this can only be achieved by making UKSPF a localised, place-based fund that is accountable to local people and places.
4.112 Councils and combined authorities should drive the design, prioritisation, commissioning and oversight of the UKSPF, which should be allocated in line with local need, deliver locally determined outcomes and support the move towards a single pot for growth funding that is long term. The Government has said the UKSPF will be at least the same amount as the current European Structural and Investment Fund (ESIF) programme. It should match the amount of any other domestic or European funds that are being included in the UKSPF.
4.113 The Government must bring forward proposals for the UKSPF at pace, co-design the fund with councils and combined authorities and underpin local efforts to drive economic recovery in the medium-long term.
Public notices
4.114 Councils are currently legally required to publish public notices in local newspapers. The decline in readership of local newspapers has meant that many residents do not have the opportunity to comment on local planning and licensing decisions. As a result, councils are spending in the order of up to £20 million on public notices that have very limited reach. In our digital age, there are more efficient and effective ways to share information with residents. We call on the Government to lift this requirement to improve information to residents at no cost to the public purse.
4.115 This would support the Government’s planning agenda of giving residents more of a say in their local area over planning decisions and the digital agenda, making access to information easier and faster. There are numerous examples, from pilot projects, of more effective ways to share information about planning and licensing, many in partnership with local newspapers. The relaxation of the rules during the pandemic, arising from limited access to local papers, showed that this could work well as a permanent flexibility.
Great places to live
Housing and planning
Delivering affordable housing
5.1 Investment in new housing supply of all tenures, from both the public and private sector, has an important part to play in a shared local and central government ambition to stimulate economic growth. New homes add important value to our economy, delivering £47 billion of output in 2019, of which 15 per cent was delivered by the public sector.
5.2 The response to COVID-19 by key workers, an excess of one million households on council waiting lists, and almost 93,000 households in temporary accommodation also provide a powerful call to action to significantly scale-up the supply of low-cost homes to rent and to buy, right across the country.
5.3 Councils already play a vital role in the supply of housing as planning and housing authorities, through direct delivery, partnerships with house builders and registered providers, and as providers of homes for the most vulnerable.
5.4 Planning for post COVID-19 activity provides an opportunity for local government to realise its potential to do much more and councils are uniquely placed to deliver more new homes than the country has seen in a generation.
5.5 Analysis undertaken in 2019 showed that councils were planning to build more than 77,000 homes in the next five years. To deliver that generational step-change councils will need increased local flexibilities and government investment to significantly expand their housebuilding programmes.
5.6 The Government has now launched its £11.5 billion Affordable Homes Programme which will be delivered from 2021 to 2026. With only around 4 per cent of the current 2016-21 Shared Ownership and Affordable Homes Programme being used to fund homes for social rent, the Government should increase the focus on this tenure in the new programme. This also needs to include increased grant levels per home to maximise the number of viable schemes. Homes for social rent are likely to become increasingly important in delivering new supply should economic conditions result in a downturn in consumer demand or ability to buy home ownership products. A step-change in the delivery of social rented homes would also deliver long-term savings in public borrowing via lower rents and reduced housing benefit spending, with research showing that each new social home would generate a saving of £780 per year in housing benefit.
5.7 With previous research for the LGA and partners also showing that investment in a new generation of social housing could return £320 billion to the nation over 50 years, there is a strong argument for countercyclical national investment in council house-building to help manage the economic impact of COVID-19.
5.8 To ensure people have the right access to a mix of housing, councils must also be able to retain 100 per cent of Right to Buy receipts and be given the flexibility to set discounts locally in order to invest in new and existing stock. While Right to Buy has helped many families get on the housing ladder, the current policy, including the restrictions around the use of Right to Buy 1-for-1 receipts, is a barrier to the delivery of replacement homes sold under the scheme.
5.9 The size of the nationally-set discount has led to a surge in the number of homes sold under Right to Buy – with 79,119 homes sold between 2012/13 and 2018/19. With councils only able to use a third of each retained Right to Buy receipt to build a replacement home, they have only been able to replace around a quarter (21,720) of these homes sold in the same period.
5.10 Councils should be given flexibility to increase the proportion of Right to Buy receipts that can be used to fund replacement homes from 30 per cent to a level that is suitable and is related to their financial models, need and place-making ambitions. The time limit for spend of Right to Buy receipts should also be extended to at least five years and councils should able to combine receipts with Homes England and other funding streams.
Unlocking land for development by councils
5.11 The cost of land for development can be prohibitive for councils and they often cannot compete against private developers and landowners. The physical availability of land, and predominance of small sites are also considered as barriers to development by councils.
5.12 We need to build on the success of One Public Estate (OPE) phases one to eight, which included two rounds of the Land Release Fund (LRF). These cost-effective interventions have seen surplus public land repurposed for housing, and, importantly, have enabled new homes to be delivered at pace. By March 2020 the OPE programme had delivered over £370 million in capital receipts for local and central government asset owners, realised over £65 million in reduced running costs, released land for over 14,000 homes, and supported over 23,000 jobs.
5.13 However, activity to release and repurpose public sector land would be far more effective if it could be planned and delivered through a longer-term programme approach, as opposed to the current process where significant OPE programme team resource is used each year to bid for further funding. A three-year funding award would enable the OPE programme to use a greater proportion of the public funding it receives on supporting project delivery.
5.14 Similarly, councils and other public bodies would be more assured to plan and develop a solid pipeline of projects with the certainty of a three-year programme of funding.
5.15 We are calling for a three-year investment programme in further phases of the One Public Estate (OPE) programme, to include further rounds of the Land Release Fund (LRF).
5.16 We are also calling for councils to be given new flexibilities to acquire public land identified as surplus or redundant by the current public sector owner in their area, to provide public facilities, including housing, at the valuation determined by the district valuer based on current use.
Planning
5.17 The pandemic has also highlighted health inequalities due to insufficient access to green space and poorly designed homes and places. A key part of the recovery is therefore the delivery of quality homes and the supporting infrastructure to create sustainable, resilient places. Councils need to be supported and properly resourced to make locally-led planning decisions for their current and future residents.
5.18 This includes having the ability to set planning fees locally. Taxpayers currently subsidise nearly £180 million per year to cover funding shortfalls. These fees should also help to cover the cost of wider planning functions to ensure that these can continue to support the decision and plan-making process.
5.19 It is unlikely that a radical overhaul of the planning system as outlined in the Planning for the Future White Paper will support the Government’s ambitions to build 300,000 homes a year in the places where they are needed, or the much needed 100,000 social homes a year, and will undermine community trust. With nine in 10 planning applications approved by councils, and more than a million homes given planning permission in the last decade not yet built, it is clear that it is the housing delivery system that is broken, not the planning system.
5.20 Reforms that restrict the capacity for councils to plan for high quality development will also exacerbate the very issues the Government wishes to address, including restricted and unaffordable housing supply, growing inequality, the need to grow our green skills and economy, and improving our health and wellbeing. As we move into economic recovery, we need developers to have the confidence to invest. This requires stability and certainty in planning underpinned by the appropriate resourcing and funding.
5.21 Should the Government take forward the proposals as outlined in the White Paper, this will result in long-term fundamental structural changes to the planning system in England. This will inevitably have significant cost implications from day one of their introduction as councils make the transition from the existing system to the new system. Any new burdens introduced for councils as they implement any new system will need to be fully funded, and the Government will need to ensure that councils have access to the right capacity, skills and training support.
5.22 In particular, it will be vital that councils are involved in the design of any new system for securing developer contributions for infrastructure and affordable housing. It is unclear what impact the proposed new Infrastructure Levy will have on the overall level of developer contributions and their distribution across the country. However, there is a risk that the huge variance in market value of developments within and across housing market areas, could result in differential capacity of local areas to benefit and fund local infrastructure need and secure affordable homes.
Regulatory services and environmental health
5.23 The local response to the pandemic has highlighted the importance of critical regulatory services that have too often in recent years been hidden from wider general awareness, despite the vital contribution they make to creating safe places to live where legitimate businesses can thrive.
5.24 The versatility and value of local regulatory services such as environmental health and trading standards, and the people working within them, has been demonstrated by their work on a range of issues including business closures and enforcement, COVID-19 compliance and health and safety, contact tracing and many other aspects of the response to which individual officers have contributed.
5.25 However, as we had already been warning prior to the pandemic, in many places, councils’ regulatory services are at tipping point:
- significant budget cuts as a result of reductions in local government funding, alongside the need to protect services such as adult social care and children’s services, have led to significant reductions in officer capacity and a reduction in services
- at the same time the number of statutory responsibilities being placed on these services has increased, adding to the pressure on already stretched services.
5.26 Even before the pandemic, this was not sustainable and reduced councils’ ability to protect their communities – but COVID-19 has brought into sharp focus the importance of maintaining resilience in services that help to keep us safe.
5.27 The Comprehensive Spending Review is the right time to begin to address the challenges faced by council trading standards and environmental health services, among others. First and foremost, it is an opportunity to address the funding shortfall and provide the resources needed to maintain these vital public protection services over the spending review period, as councils continue to lead local work to tackle COVID-19.
5.28 However, wider changes are needed to ensure services are placed on a sustainable footing beyond the CSR period.
5.29 New models of funding can help to support services while reducing the burdens on taxpayers, and the Government should therefore progress the recommendations of the Regulatory Future review on implementing proportionate charges on the businesses that benefit from regulation – a principle that is already accepted in our licensing frameworks – in particular following the polluter pays principle. This can also help in addressing challenges with the pipeline of officers entering the workforce by supporting a sustainable funding model that can build future resilience, so that services with a key role to play in enabling the recovery from COVID-19 and supporting businesses as we move through the EU transition period are safeguarded into the future
5.30 We have drafted a joint submission with the Chartered Institutes of Trading Standards (CTSI) and Environmental Health (CIEH) which outlines our call for the Comprehensive Spending Review to address the challenges faced by council trading standards and environmental health teams in more detail.
Tourism and visitor economy
5.31 The visitor economy is one of this country’s fastest growing economic sectors. The cost of failing to invest in it now will have a significant impact on the economy and unemployment levels. The critical success factors for unlocking further growth – skills, transport, digital infrastructure and business support, are all policy areas where the evidence suggests devolution will enable better and more efficient decisions to be made for the visitor economy, particularly in coastal and rural areas.
5.32 We believe there is a clear need for direct investment in the tourism sector of at least £1 billion, in addition to the extension of existing packages of support. The new £1.57 billion cultural and heritage fund announced on 5 July should also complement a comparable investment in tourism, given the close inter-relationship of these sectors.
5.33 Different areas will have different levels of need for investment, with some areas, such as coastal communities, more at risk of the impact of COVID-19. A place-based and collaborative approach will need to be adopted by national partners, including Arts Council England, Historic England and VisitEngland.
5.34 In the short term with a shortened and smaller summer season affected by COVID-19, followed by an end to government support in October, it is important to avoid a cliff-edge. The Government should work to maximise 2020’s income by extending the season into autumn and winter. Councils and combined authorities have suggested a variety of ways this can be achieved:
- Visit Britain/England to devolve budget and/or control of how regions are promoted to focus on autumn and winter, as well as periods beyond this
- out of season events development funds and relaxation of restrictions on holiday parks and resorts to allow out of season operation
- a specific support plan for the tourism and hospitality sector to see it through until March 2021, and beyond that, funding to deliver the tourism sector deal priorities.
5.35 Over the Comprehensive Spending Review period, we are calling on the Government to:
- Introduce a funding programme, worth at least £100 million, that builds on the work of the Cultural Destination Programme, Great Places Scheme, and Discover England Fund which enables arts and culture organisations to increase their reach by working with the tourism sector. Councils with seaside resorts are likely to be some of the hardest hit during the pandemic. It is crucial local authorities have every opportunity to support this sector.
- Provide freedoms and flexibilities around different funding streams which would allow the refocus of existing funding to support place-based recovery, led by growth boards. Working with other departments and expanding criteria and objectives for the Cultural Development Fund, high streets funding, and Stronger Towns funding, this could support councils to convert and adapt buildings, including high street premises, into studios to facilitate the creative industries contribution to recovery.
- Make sure the UKSPF explicitly acknowledges cultural, creative, heritage and visitor economy objectives in addition to supporting wider economic growth through strategically planned infrastructure investment, including broadband and digital connectivity.
- Conduct a rapid review of destination management organisations to ensure they are appropriately structured and resourced to deliver on marketing and business support needs. There had been variable performance even before COVID-19 and, while some have provided invaluable support to businesses recently, others have had to furlough staff from financial necessity. Effective marketing and business support to tourism businesses and potential visitors will be critical in the months ahead.
- Expand in number and scope Tourism Zones, announced as part of the Government’s Tourism Sector Deal, with appropriately scaled funding levels, and brought forward as soon as possible. This should include innovative options for raising finance, building on proposals from the Cultural Cities Enquiry, the option of a tourism levy, and business improvement districts. Receipts from taxation should be ringfenced for investment in the area that raised the tax. Possible expenditure should include council services supporting the visitor economy (such as the public realm and parking), tourism market intelligence and out of season marketing in order to ensure industry buy-in. The overall number of zones should be increased to 40, with £40 million funding provided to kickstart their work.
Culture and creative spaces
5.36 Government statistics show that in 2018 the UK’s creative industries contributed more than £111 billion to the UK economy, equivalent to £306 million every day or £13 million every hour – more than the automotive, aerospace, life sciences and oil and gas industries combined. This was a 7.4 per cent increase on 2017, so growth in the creative industries was more than five times larger than growth across the UK economy as a whole.
5.37 In addition, creative industries have increased their combined contribution to Gross Value Added (GVA) by 43.2 per cent in current prices since 2010.
5.38 More than two million people work in the UK’s creative industries and, before the COVID-19 crisis, the sector was projected to create another million jobs by 2030. Jobs in the creative economy tend to be higher value, better paid and be more skilled than the average in the wider economy. However, to sustain this requires a talent pool to be developed and maintained.
5.39 Parts of the creative industries have been hit harder by lockdown and the ill-effects will last longer than for other sectors of the economy. Those businesses that rely on attracting audiences or visitors will be the last to return to normal operations with no clear picture of when that might be. If we value the sector, we must all work together to secure its future.
5.40 As well as supporting the sector in its time of need, we must also consider the part creative enterprises and freelancers will have in helping us lead the nation’s recovery. These businesses and individuals are naturally creative, adaptable and resilient. We must harness this creativity and the innovation inherent in the sector to take on the challenges of a post-COVID world, generating jobs and investment in local economies.
5.41 We need a place-based approach to post COVID-19 cultural sector recovery. Each area faces different conditions, has lost different elements of its local ecosystem and will be in a different starting point for recovery. Councils are the local leaders of place and best placed to coordinate recovery. By ensuring councils are at the top table for discussions – including the new Cultural Renewal taskforce and the Tourism Industry Council, their resources and expertise can be harnessed to maximise impact. Arts Council England’s new strategy recognises this approach, and the Department for Digital, Culture, Media and Sport (DCMS) should support Arts Council England to return to its delivery plans as soon as is feasible.
5.42 Culture drives footfall in high streets – the West End remains empty without the theatres. For example, Liverpool city centre is experiencing a 40 per cent reduction in footfall due to their absence. Central and local government needs to collaborate to revive and drive the cultural recovery, with its proven impact on GDP (joint fastest growing economic sector, with tourism, prior to COVID-19).
5.43 Leadership is critical in achieving this. Councils and combined authorities should be supported by Arts Council England with £400,000 in revenue funding to develop more cultural compacts, as identified by the sector for the sector. As shown by the pilot in Lancaster, this is a proven approach which can deliver.
5.44 The business case developed by the Leadership for Libraries Taskforce, convened by DCMS and the LGA, demonstrated that makerspaces are a swift, cheap, and popular way of bringing creativity and innovation into communities that have previously had few creative outputs. 17.3 million people in the UK lack the essential digital skills for life or work, which makes the provision of public access computers in libraries, and the support provided to train people in the skills to use them, more vital than ever. A £30 million capital funding investment in libraries to develop a network of makerspaces and public access computers would support our country’s recovery, close the digital skills divide in many of our most deprived areas, and grow entrepreneurs and innovators in every council area.
5.45 We are calling for a rapid rollout of the announced next tranche of business and intellectual property centres. These centres have proven their ability to reach and support a broader and more diverse range of entrepreneurs and will be critical to re-establishing a thriving ecosystem of small businesses and freelancers. Alongside this, a specific cultural and creative support offer should be developed, similar to Arts Council England’s digital champions.
5.46 The Government should provide councils with additional funding of £500 million to invest in supporting social prescribing facilities, including leisure centres and libraries which support community activities. Building on existing work to develop social prescribing models, DCMS should work with the National Academy for Social Prescribing to ensure that cultural organisations are funded to deliver wellbeing outcomes, resulting in a more resilient and productive workforce. While the National Academy is funding link workers, we need investment in providers to ensure they have the capacity, skills, and know how to deliver the improvements to individuals, and the savings to the health service, that are needed for our nation to thrive.
5.47 Finally, making £100 million capital funding available to convert disused retail units on the high streets into creative studios would enable creative industries (worth £111 billion GDP) to thrive and drive footfall to high streets by offering chance to grow entrepreneurs and innovators for the future by delivering 3D printing, coding and display spaces for creative experimentation. This must be coupled with the planning powers needed to curate high streets, as was done by removing permitted development rights from theatres and performance venues, protecting them from inappropriate development and preserving them for the community.
Parks and green spaces
5.48 The Government has already committed to spending £2 billion in this parliament on cycling and walking. During the lockdown period, many people used their hour of exercise to enjoy our public parks and green spaces, with Sport England data showing 30 per cent of people being more active during this time.
5.49 As we invest £2 billion in active travel, we must ensure that our parks and green spaces are fully connected to these plans and also benefit from investment. Building on the success of the Green Chain Walk and Thames path in London, when connected, these spaces can make a powerful contribution to tackling obesity and getting more people active.
5.50 The pandemic has hit those from more deprived backgrounds and the BAME community hardest, whether that be through deaths, digital poverty or a lack of accessibility to parks, private gardens and green spaces to exercise. Research by PHE has revealed that the most vulnerable do not have equal access to green space.
5.51 The way in which parks are funded has changed significantly over time. Since 2010 core council funding has reduced by over £250 million and the reliance on commercial income, fees and charges has increased. This income has dropped to near zero during the pandemic.
5.52 Parks provide a cheap and cost-effective way to get people active, reduce obesity, boost mental wellbeing, and strengthen immune systems. At the same time, they can help act as green corridors for wildlife, refuges for pollinators, act as sustainable drainage systems, and mitigate the impact of air pollution.
5.53 Small scale, affordable initiatives to help the nation’s parks and green spaces recover and flourish can add up to a major impact on our nation’s health, environmental footprint, and resilience.
5.54 We are calling on the Government to introduce a local, flexible £500 million Green Parks Fund to help unlock such initiatives, with a £450 million capital element and an ongoing revenue commitment of around £50 million.
Table 5.1. Examples of initiatives to improve parks and green spaces that could be funded through the Green Parks Fund
|
Initiative |
Details |
Estimated cost |
|
Parks Activation funding |
Creating jobs for a new breed of ‘community park rangers’ to help ‘activate’ our green spaces and deliver more community health focused outcomes such as green prescriptions, activities and volunteering, linking into the more hard-to-reach sections of society who need more reassurance to use our green spaces. |
£30 million revenue funding
|
|
Meadow creation |
A transformation fund for the creation of pollinator-rich grassland meadows on current areas of close mown grass in parks and open spaces, as referenced in the 25-year environment action plan and Defra’s bees needs campaign. |
£10 million capital funding
|
|
Playbuilder + |
Capital funding for the refurbishment of play facilities to encourage active play as part of the anti-obesity strategy. Not just confined to children’s play equipment but also including things such as exercise equipment for all ages along with removing any accessibility barriers. |
£300 million capital funding (based on 10 play areas per authority) |
|
Quality Parks (in partnership with Green Flag Award) |
Capital and revenue funding to transform parks in target wards into Green Flag Quality Standard green spaces delivering community cohesion, health and wellbeing, or climate mitigation outcomes. |
£50 million blend of capital and revenue funding (based on 100 parks) |
|
Green Space Protection (in partnership with Fields in Trust) |
A national campaign to protect existing green spaces with funding that covers legal and dedication costs, allowing landowners to donate to our nation’s health and green future in a way comparable to the post-war donations of historic buildings to what became the National Trust. |
£1 million revenue funding
|
|
Emergency Parks Fund |
Emergency revenue funding to support parks through the current challenges, including emergency repairs to existing equipment and paths to embed and enable active habits during lockdown to be maintained. |
£500,000 revenue funding |
Initiative Details Estimated cost
Parks Activation funding Creating jobs for a new breed of ‘community park rangers’ to help ‘activate’ our green spaces and deliver more community health focused outcomes such as green prescriptions, activities and volunteering, linking into the more hard-to-reach sections of society who need more reassurance to use our green spaces. £30 million revenue funding
Meadow creation A transformation fund for the creation of pollinator-rich grassland meadows on current areas of close mown grass in parks and open spaces, as referenced in the 25-year environment action plan and Defra’s bees needs campaign. £10 million capital funding
Playbuilder + Capital funding for the refurbishment of play facilities to encourage active play as part of the anti-obesity strategy. Not just confined to children’s play equipment but also including things such as exercise equipment for all ages along with removing any accessibility barriers. £300 million capital funding (based on 10 play areas per authority)
Quality Parks (in partnership with Green Flag Award) Capital and revenue funding to transform parks in target wards into Green Flag Quality Standard green spaces delivering community cohesion, health and wellbeing, or climate mitigation outcomes. £50 million blend of capital and revenue funding (based on 100 parks)
Green Space Protection (in partnership with Fields in Trust) A national campaign to protect existing green spaces with funding that covers legal and dedication costs, allowing landowners to donate to our nation’s health and green future in a way comparable to the post-war donations of historic buildings to what became the National Trust. £1 million revenue funding
Emergency Parks Fund Emergency revenue funding to support parks through the current challenges, including emergency repairs to existing equipment and paths to embed and enable active habits during lockdown to be maintained. £500,000 revenue funding
Community safety
Domestic abuse and COVID-19
5.55 Domestic abuse can have a long-term and devastating impact on families and particularly children. It is the most common reason for children to be classed as ‘in need’ and allocated a social worker. It can take the form of psychological, physical, sexual, emotional or economic abuse, and occur in a wide range of domestic settings.
5.56 Unfortunately, the emergency response to the pandemic has meant that perpetrators of domestic abuse have been more likely to be at home with the victim. A joint investigation by Panorama and Women’s Aid found someone called the police for help about domestic abuse every 30 seconds in the first seven weeks of the UK’s lockdown. The investigation found that three-quarters of victims said the lockdown had made it harder for them to escape their abusers.
5.57 It will take time before we are able to fully understand the impact of how the nationwide shutdown in response to COVID-19 has affected victims of domestic abuse. The need for comprehensive domestic abuse services, and effective perpetrator interventions, could never be more crucial. These devastating accounts of domestic abuse demonstrate the importance of all partners and organisations helping to prevent and eliminate this appalling crime.
5.58 Long-term, sustainable funding is needed in order to transform the response to domestic abuse. The social and economic cost for victims of domestic abuse in England and Wales were estimated to be approximately £66 billion a year (in year ending March 2017). While the £66 billion estimate of the costs of domestic abuse appears large, it is likely to be an under-estimate.
5.59 Whilst the funding that the Government has announced in order to tackle domestic abuse during COVID-19 is welcome, we now need a long-term settlement as these one-off, short-term funds do not provide consistency or sustainability in the sector.
5.60 We are calling on the Government to provide long-term and sustained funding for early intervention and prevention programmes and wider community-based domestic abuse support. This funding needs to be similar in scale to the Youth Endowment Fund which is £200 million over 10 years. This should include investment in perpetrator programmes, which is why we are calling on the Government to introduce a National Domestic Abuse Perpetrator Strategy.
Domestic Abuse Bill
5.61 It is positive that the forthcoming Domestic Abuse Bill introduces important measures which will help to raise awareness of domestic abuse and will go some way to providing additional support to domestic abuse victims and helping to challenge perpetrators’ behaviour.
5.62 The Bill seeks to place a statutory duty on many local authorities to provide support to victims of domestic abuse and their children within refuges and other safe accommodation, in addition to other measures.
5.63 It is important to state that any new statutory duties require comprehensive and long-term funding. A statutory duty to deliver domestic abuse accommodation support and services will not be effective without a clear commitment from Government to provide adequate and sufficient funding.
5.64 It is therefore welcome that the Government has confirmed that councils will receive appropriate financial support to meet the proposed new duty, and that final decisions on funding will be made as part of the Comprehensive Spending Review.
5.65 We look forward to providing input to the full New Burdens Assessment which must be available ahead of the new duty coming into force. We believe that domestic abuse funding needs to meet the following tests:
- The new funding should fully account for any increases in demand for services.
- Currently, there is a variety of different funding streams for domestic abuse specialist services. Often these are one-off, short term grants that do not allow for long-term planning or consistency in service. In order to transform the response to domestic abuse, a joined-up approach needs to be implemented to unlock a broad range of support packages available to support victims of domestic abuse and intervene with perpetrators to change and prevent their behaviour.
- We are concerned that only councils will be subject to a statutory duty, yet funding for domestic abuse services tends to be routed to other bodies. For example, the majority of the Government’s COVID-19 funding pots targeted at domestic abuse were only made available to frontline services (outside councils) or police and crime commissioners (PCCs).
Modern slavery
5.66 Estimates of the number of victims of modern slavery in the UK range from 13,000 to more than 130,000, with the overall costs to UK society of modern slavery estimated to be between £3.3 billion and £4.3 billion.
5.67 As highlighted by LGA guidance on modern slavery, developed in conjunction with the Office of the Independent Anti-Slavery Commissioner, councils have a role to play in disrupting slavery and identifying and supporting victims.
5.68 Latest statistics show the number of council referrals of suspected child victims of modern slavery in England to the National Referral Mechanism (NRM) – the UK’s framework for referring and supporting victims – has risen from 127 in 2014 to 1,971 in 2019, an increase of 1,452 per cent. Referrals of adult victims rose from 28 in 2014 to 190 in 2019, an increase of 579 per cent.
5.69 This spiralling rate of modern slavery referrals is being fuelled by an increasing awareness of the exploitation of young people by county lines drugs gangs and of other forms of modern slavery.
5.70 It is further evidence of the huge pressure on children’s services, but the rising number of adult victims is also adding to demand for housing and adult social care support. However, there can sometimes be challenges in providing supporting to adult victims in particular, with councils not set up or required to provide the specialist support that victims need, issues over eligibility criteria, and pressure on key services.
5.71 Despite the increasing number of victims of modern slavery, no specific funding has ever been given to councils to support work on modern slavery, either in terms of the disruption activity that could be supported by regulatory services if given greater resources, or in terms of the growing number of victims seeking support from councils. With the Home Office currently reviewing the National Referral Mechanism to ensure its sustainability into the future, the Spending Review is an opportune time to assess the level of funding required to support victims of modern slavery.
5.72 With adequate funding, councils can help disrupt and tackle the crime through regulatory services and provide support to the growing numbers of victims going into and coming out of the NRM.
Countering extremism
5.73 The past few months have seen the emergence of a number of extremism and cohesion challenges, with extremists seeking to exploit issues to extend their reach and garner support.
5.74 We expect that extremists will continue to use the post-COVID landscape to further their narratives – economic decline and rising inequality (or perceptions of these) in particular have traditionally provided fertile territory. Councils are increasingly concerned about the need to respond effectively and build resilience to emerging tensions and threats from hate crime and radicalisation; it is vital that continued investment in prevention and resilience work, including integration, counter-extremism and Prevent initiatives, is secured.
5.75 Over the last four years the Special Interest Group on Countering Extremism (SIGCE) has been a significant and agile force in supporting both local and national government’s efforts to counter extremism, tackle hate crime and help counter the ideology that can draw individuals into terrorism, including through deepening understanding of activists, ideology and tactics, and in developing and sharing practice around nurturing relationships with and mobilising local residents, communities and the voluntary sector, disrupting extremist activity, community engagement and resilience building. Over the last few months the network has continued to bring together councils from both counter-extremism ‘supported’ areas and non-supported areas, to assist councils facing increasing extremism and cohesion pressures during the pandemic, to share learning and provide bespoke direct support to areas facing specific threats. Central government funding from April 2020 has not been secured and the SIGCE’s future is currently uncertain. We believe it remains key to addressing rising tensions in many areas, and in supporting wider efforts to help prevent terrorism, which we are concerned will be growing issues for local areas in the coming months and years.
5.76 We anticipate that Government will shortly consult on a new Protect Duty to improve safety and security at public venues and spaces. We expect that this will have implications for local authorities; any new burdens introduced for councils as part of a new duty must be fully funded.
Fire and rescue
5.77 A decade of austerity has had a significant impact on fire and rescue services (FRSs), resulting in a real-terms cut of 29 per cent in standalone fire and rescue authority (FRA) budgets and a consequent decline in staff numbers over that period.
5.78 Despite this, the HM Inspectorate highlighted in their first national report significant strengths in the commitment of staff, dedication to protecting life and property, life-saving prevention initiatives, highly skilled emergency response and the admiration in which services are held by the public.
5.79 During the COVID-19 pandemic, FRSs have further demonstrated their ability to support other agencies in times of crisis, utilising the wide geographical spread of local resources and high levels of public trust to support vulnerable people in their communities. This also shows how the sector is well-placed to respond to other emergencies, such as flooding.
5.80 Many services already have some capacity to respond to these incidents, however, support for a consistent approach based on risk would require capital investment.
5.81 FRSs also face a wide array of cost pressures which affect different areas in different ways:
- The renewal of the national resilience (New Dimensions) assets is estimated to cost £100 million, in addition to the implementation of the Emergency Services Network, the roll-out of which has been delayed, increasing the costs of the programme. Neither of these costs should be placed on FRA budgets.
- With the majority of authority fire service budgets being made up of workforce pay and pensions, pay inflation is a major pressure across the sector. This is addressed in more detail below. A review should be conducted of the sustainability of the retained duty system and the Government should commit to supporting FRAs in funding alternatives if necessary.
- Improvement activity is also a significant area of work which services are undertaking following the publication of the Grenfell Tower Inquiry Phase 1 report (GT1) and the first Her Majesty's Inspectorate of Constabulary and Fire & Rescue Services (HMICFRS) State of Fire report. Areas of focus include protection activity, culture change, innovation and technology, and governance.
- In 2020/21, the sector was granted £20 million for enhanced protection activity and a further £10 million for the implementation of the GT1 recommendations. This investment needs to continue over the Comprehensive Spending Review period to ensure the continued improvement of protection teams and to retain capability.
- New burdens being placed on the FRS through the introduction of new legislation also need to be funded. The Government estimates Fire Safety Bill ongoing costs to reach £30.3 to £44.7 million per year depending on the option selected in the current consultation on fire safety. In addition, the Government’s impact assessment on the Building Safety Bill estimates the FRS will see a £9 to £15 million increase in FRS staffing costs. As the impact assessment does not break down all costs by the individual elements of the proposed regulatory regime, the full cost of the Bill to FRS remains unclear, but training needs that will arise from the Bill need to be taken into account.
- On top of these already existing pressures, COVID-19 has had a significant impact on funding due to the reduction in council tax and business rates collections. The impacts of the pandemic and subsequent lockdowns are not yet fully understood, but the current collated data from billing authorities forecasts a national loss of £55.6 million in 2020/21, the equivalent of 1,300 firefighters or around 6 per cent of the wholetime workforce.
5.82 FRSs are resourced to risk, meaning that the services must have the ability to deal with large scale emergencies and/or a range of smaller incidents all occurring simultaneously and over an extended duration. To provide this, services must be able to operate resiliently and across borders.
5.83 To at least maintain the current activity and the current firefighter numbers, an inflationary increase to fire funding will be needed. Further investment and the flexibility to increase the council tax precept (£5) will be needed to build on existing improvement activity, particularly around technological innovation and cultural change.
5.84 Governance is a central pillar of the fire sector and elected members have a key role to play, setting the policy direction for their services and challenging them to make improvements where necessary. Sector-led improvement is a key element of improving the capabilities of elected members to fulfil this responsibility. Home Office should work with the LGA on a £120,000 programme of member development and support the development of a programme of activity around principles of good governance and decision-making.
Fire and rescue pensions
5.85 Pensions are a significant cost pressure on FRA budgets, arising from both employer contributions and managing and administrating the scheme.
5.86 FRAs are deemed to be the scheme manager for the Firefighters Pension Scheme and as such are responsible for the funding of administration and management of the scheme. These costs are met solely from their core funding.
5.87 It is expected that the implementation of the Age Discrimination Remedy, known as the McCloud/Sargeant judgement, as well as implementing the more short-term immediate detriment guidance recently issued by the Home Office, will result in significant additional costs to FRAs, their administrators and software developers, resulting in an estimated additional new burden of 50 to 75 per cent of current costs. This amounts to approximately £3.5 million.
5.88 The administration and software requirements to facilitate a second options exercise to implement Matthews (the case to allow retained Firefighters employed before 2006 the ability to join the 2006 scheme as Special Members for service before 2000) is also expected to be a significant new burden, estimated at 50 per cent of current costs, or £2.5 million.
5.89 Employer contributions from 2022 will be determined by the 2020 valuation, which will be impacted by any SCAPE rate adjustments and the cost of McCloud and Sargeant and Matthews. No information has been shared with the sector on the directions that will shape these costs, but given central estimates of £2.5 billion per year for all schemes, this will have a significant impact.
5.90 Employers have also recently received guidance direct from the Home Office instructing them to fund the additional employer contributions for any member who wishes to retire and receive benefits as if they had been a member of the legacy scheme. This creates an immediate unbudgeted funding pressure:
- the current difference between Fire Pension Scheme (FPS) 1992 and FPS 2015 employer contributions as set by the 2016 valuation is 8.5 per cent
- the difference between FPS 1992 and FPS 2015 employer contributions set by the 2012 valuation is 7.4 per cent.
Fire and rescue pay
5.91 Firefighters have been subject to pay freezes and below-inflationary increases for many years and the sector is under significant pressure from unions to deliver a large pay rise in 2020.
5.92 The National Employers’ position, following consultation with chairs and chief fire officers, is that any pay rise beyond 2 per cent in 2020/21 would have been unaffordable for the sector without additional government funding. We estimate that a 2 per cent increase would cost the sector at least £25 million per year, representing more than 1 per cent of total funding for the FRS. Additional funding is needed for subsequent years’ pay awards in order to secure agreement and the ambition for reform set out below.
5.93 Beyond 2020/21 it is expected that the pressure for pay awards above 2 per cent will continue to increase. Any agreements will be subject to the national negotiating arrangements through the National Joint Council for Local Authority Fire and Rescue Services, but affordability remains a major issue.
Reforming the fire service
5.94 The nature of risks that the FRS helps manage has changed over time. The Grenfell Tower fire has again highlighted the high expectations of the public in terms of service delivery.
5.95 FRSs can also play a greater role in the wider regulatory environment, all of which needs to be seen in the context of other drivers for improvement.
5.96 During 2020 a major piece of work, ‘Fit for the Future’, was undertaken in partnership by the LGA, National Employers (England) and the National Fire Chiefs Council (NFCC) to establish a common picture, or vision, for the future of FRSs in England.
5.97 This review also supports the sector’s and government desire to deliver reform, including reform of firefighters’ roles in line with ongoing and emerging objectives.
5.98 To achieve the ambition of Fit for the Future, it is clear that the sector would need to be supported and sustained by an increase in government funding. Current estimates on pay alone are in the region of an increase of 15 per cent over the three years in order to achieve a negotiated settlement, with each percentage point increase in pay worth around £12.5 million per year.
5.99 To increase expenditure on pay to the level required over the CSR period to deliver Fit for the Future is undeliverable from existing budgets without impact on numbers employed and service delivery. For context, each percentage increase above affordable levels would be equivalent to over 300 firefighters.
5.100 To strengthen delivery of reform and as part of Fit for the Future, the LGA and NFCC have identified a need to put in place a group of improvement specialists tasked with supporting the implementation of reform at the local level within FRSs in England. Such implementation support will be a vital part of securing success. It is recognised that both parties need government funding in order to progress this initiative. From an LGA perspective this will require funding to put in place increased employment relations support for FRSs of £200,000 a year.
Building safety
5.101 Local authorities are generally being denied access to the building safety remediation funding announced earlier this year in relation to dangerous non-aluminium composite material (ACM) cladding. On the basis of experience gained from the remediation of ACM cladding to date the LGA has estimated that the £1 billion provided for the remediation of non-ACM cladding will be around a third of the total cost of replacing dangerous non-ACM cladding. The Government has as yet offered no legal justification for operating the fund on a first-come-first-served basis or for denying councils access to the fund.
5.102 Earlier this year the LGA commissioned research from Savilles which estimated that the total costs to deliver Building Safety Standards across the entire HRA council housing stock are estimated at £8.1 billion over a 10 year period, with the majority of the investment taking place in the first five years, to achieve full compliance with the highest possible standards, including the installation of sprinklers and compartmentation. Achievement of compliance with standards as currently set out is estimated to be a total of £2 billion over the same period.
5.103 At the same time the Fire Safety Bill may require councils to renew all fire risk assessments to cover external wall cladding systems. This is likely to be expensive as there is a severe shortage of qualified surveyors willing and able to undertake the work. The commencement of this Bill and its relationship to the supply of skilled assessors is under discussion with officials at present.
5.104 In addition to remediation costs, councils face ongoing costs in employing building safety managers, providing safety cases and other costs under the new regime. Where private landlords are able to increase rents to cover these costs, councils’ ability to do so is limited by Government and statute.
5.105 In addition to the costs for FRSs arising from building safety reform, the Building Safety Bill Impact Assessment estimates increased staffing costs for local services, such as building control, planning and environmental, of £10 to £22 million.
5.106 Some of these costs will be offset by the cost-recovery mechanisms set out in the Bill, but the significant costs of recruiting and upskilling staff are unlikely to be included in the estimate above and we are concerned whether the approach to cost recovery will result in all regulatory costs being covered.
5.107 The extent to which upskilling will be required to deliver the ambition of the Bill is as yet unclear, but it is clear that it will be vital to making the Bill a success and costs to councils will include training for building control staff. Uncertainty over the future of some of the proposals in the Bill as a result of the conflict between its provisions and the Planning for the Future White Paper makes estimation of the full cost to councils as regulators more difficult.
5.108 A failure to cover costs will deter regulators from taking enforcement action and undermine the effectiveness of the Bill (as had been the case with existing legislation).