This case study forms part of the publication, Bespoke support for people with learning disabilities and autistic people, an evaluation on the impact consequence for local authorities and councils of delivering bespoke support to autistic people and people with a learning disability, including people who have been detained under the Mental Health Act (or at risk of being detained).
There’s a balance between sharing Paul’s story and respecting his privacy. You’ve got to consider the trauma involved. People are revisiting their trauma each time they tell their story."
Paul was in five different psychiatric hospitals over 19 months. Having said that, he’s been institutionalised since he was 10 years old, so he has spent most of his life in institutional settings of some form. He started off in a Psychiatric Intensive Care Unit (PICU), then he went to an Assessment and Treatment Unit (ATU), then he went to another PICU, then a locked rehab unit, followed by another locked rehab hospital.
Every place said they couldn’t handle him. Already what you’ve got there is completely inappropriate settings and staff who are unable to evaluate the ‘real him’. All they see is the reaction to distress and they think it means he needs to be locked up rather than try to take the distress away. I regularly took Paul out on section 17 leave by myself into the community: trainspotting, visiting a farm or having a coffee. We never had any issues at all.
It comes back to the whole business about whether you think that hospitals are appropriate places for people with learning disabilities and autism.
In Chapter 20 of the Mental Health Act Code of Practice it says that compulsory detention in an inpatient unit is rarely likely to be helpful for a person with autism because of sensory overload, the whole environment, staff who don’t know the person or who don’t have the right training. So already you’re in an environment which is never going to work. It’s thinking that hospital will work, (never mind how you’re assessing the person) which is just plain wrong.
At the ATU which Paul went into for a brief period there was another patient there who was extremely noisy. Paul couldn’t tolerate the noise and he would react to that. He would go out into the garden to get away from the noise and start throwing furniture around, because he was completely overloaded. I asked why they would even let him come to that hospital when they knew how noisy it was going to be.
If I’d known then what I know now, I’d be very vocal about hospital not being the right place for him."
When Paul came off section, he was being over-medicated and was still in hospital. Everyone went into panic mode. They said that he was going to have his own home with his own team, but it didn’t happen. The mental health team was saying things like “He won’t need his own car, will he? He can get the bus. There will be good staff and bad staff. Paul will just have to get used to the bad staff.”
Paul couldn’t manage the bus most of the time, but they just wanted to find the cheapest way of doing things…and as for having ‘bad staff!’
I realised then that this approach was not going to work. We started the process of finding another way of getting him out of hospital. We managed to find a residential home about an hour away that was split into flats and fought to have Paul discharged there.
He ended up being there for several years and completed a college course. He did well, but we still felt his needs weren’t being properly met and that the PTSD he had been diagnosed with as a result of his hospital stay wasn’t being addressed. Paul’s nights were disturbed, and he started to display signs of catatonia. Sharing space with other (sometimes distressed) people just wasn’t working for him.
We started the process of obtaining an NHS capital grant to buy Paul his own bungalow close to us. It was a long drawn-out process, but with the help of a family advocate, the wheels were set in motion. We found a great landlord in Choice Support who involved us all in finding and adapting the right property.
Then the pandemic hit, and we brought Paul home with us because we didn’t think he’d cope with being isolated in a small flat on his own without access to family for a long period of time. We didn’t know how long the restrictions would be in place. We made the decision as a family to have him at home and to try and make it work all together. The planning for Paul’s move into his new home continued while he was at home with us, and when he moved into his own place, he transitioned there from the family home rather than from the previous support provider organisation.
It went well from the start. Paul has an experienced staff team who got to know him during the transition, and they really do go the extra mile to help him.
The ‘right to deny entry’ is part of ancient housing law. If you think about it, that means that you should be able to choose your own support in your own home. For people coming out of hospital, living alone needs to be considered as something the person might need, in order to live in a bespoke environment and to move on from their trauma.
Paul is back home after all these years. He’s five minutes away from family. He’s happy. It’s going well. He’s got a good life. He’s making plans for the future and everyone’s up for facilitating it. There’s so much good stuff happening”.
Brenda- Paul’s Mum, London area
The Aurora Nexus team got involved in supporting Paul when Brenda was able to secure an NHS capital grant for purchasing a bespoke property for Paul. At this stage he was living an hour away from home. He was in a residential setting and the family recognised that he was not going to be able to get over his trauma and move on with his life while he was living there. Brenda recognised that Paul needed the opportunity to recover from his trauma, and he needed to be in his own property where the environment and the support could be tailored to him specifically.
Where the family lived, there were a few providers which could be explored, but not many. Brenda started to ask some of her connections and made introductions with Aurora Nexus from recommendations she received. Aurora Nexus was not on the approved provider list with the local authority, and to begin with it was difficult for the local authority to agree to working outside of their usual contracting arrangements. Good joint working and communication meant that all parties were able to find a solution
All of this was only made possible because Brenda led the search and the exploration of options and possibilities. There seemed to be some entrenched thinking about ‘this is not the way things are normally done’. The local authority and CCG did take some time understanding that it was possible, and how it could be implemented.
Brenda developed a specification of Paul’s housing needs, carried out all of the local market research herself, and completed the bid form for the housing part of the arrangement. All of this information was presented to the local authority, initiated by Brenda. Effectively, Brenda brokered Paul’s support herself through researching, informing herself about Paul’s rights and making connections.
Once the local authority understood how the arrangement was going to work, they were very supportive. They supported Brenda with interviewing providers and supported her with the whole planning process.
Brenda started having conversations with Aurora Nexus. Initially there were some concerns about whether the organisation could support Paul (the organisation at the time was quite small and wanted to be sure that Paul could be supported safely and well) but they carried on having conversations with the senior management team at the organisation, and there was an agreement to design a bespoke package of support for Paul.
The provider developed a proposal which was presented to the local authority and the CCG. The CCG asked some ‘random’ questions which were difficult for the provider to answer. For example, the provider wanted to connect into the local community mental health and learning disability teams to support Paul once he moved, rather than employing internal therapeutic staff (such as psychologists and psychiatrists). The CCG wanted to know why the provider was not going to provide internal clinicians as part of the support package.
Another example was that Paul required 2:1 support, and the CCG wanted to know whether the second member of staff could be paid less than the first. There was a complete lack of understanding from the CCG about how to provide person-centred support to people in their own home.
Eventually, Paul received his section 117 funding via a Direct Payment arrangement, and this enabled Brenda to contract directly with Aurora Nexus to provide Paul’s support in his own home. The Direct Payment is passed from Brenda directly to the provider and is treated like an ISF arrangement, using the budget flexibly around Paul’s support requirements from week to week.
Paul’s team liaise directly with Paul’s family to flex his support around planned activities and family events Paul wants to be involved with. There is no ‘time and task’ monitoring in terms of how the budget is spent. The provider is trusted to risk assess and provide the appropriate levels of support as required according to the activity. Some of the budget can be ‘banked’ to be used at times where higher levels of support are required.
Internally at Aurora Nexus, they focused on building the team for Paul, getting his property ready and preparing for him to move into his own place. The provider team couldn’t imagine Paul being the way he was described in the inpatient settings- the descriptions simply didn’t match with what they were seeing and how they were getting to know Paul as a person.
Gathering information about Paul and understanding how to support his needs proved very difficult. Aurora Nexus had to get the social worker involved to request information from the previous provider. There was a reluctance to share information.
The support team made a conscious effort to make reference to all aspects of Paul’s support with him at the centre. They even referred to Paul’s support service as ‘Paul’s House’ within their internal reporting systems, rather than giving it a ‘service name’. This has really helped with setting the right culture with Paul’s staff team from the beginning. This is also the case with financial reporting against Paul’s budget and support, and any communications with the local authority and CCG- all of these elements are defined as ‘Paul’s House’, and ‘Paul’s Support’.
Paul has a consistent and stable staff team. His support team are paid a slightly higher hourly rate which fits within his budget, in recognition of the skilled support they provide and the additional training they require.
It has not been easy to source specialist training, but the staff team have taken the lead in identifying what they require for their development needs in order to support Paul well and have used their initiative to build their knowledge and skills to meet Paul’s specific support requirements.
For example, Paul really likes trains and enjoys watching Thomas the Tank engine; so the staff spent some time together learning about Thomas the Tank engine and thinking about why it is a positive and important part of Paul’s life. Aurora Nexus recognise that good support is about getting the culture right. You can provide all of the right training within a classroom context, but it doesn’t necessarily translate into good support for the person unless the service is well led and managed by practitioners who understand how to set the culture in the right way for the person being supported.
They have recognised the need for trauma-informed and low-arousal support approaches, but this type of training does not come cheap, and really needs to be factored into the overall budget for the person’s support to ensure that the staff are providing support in a way which upholds the person’s wellbeing and does not add to the trauma they have already experienced in other settings.
For Aurora Nexus, they have found that the commissioning process is so important. Managing risk and being quite calm about that. Of course, there are tricky days, but everyone is allowed a bad day. The important thing is being able to have a calm conversation about it, recognise it for what it is (a bad day) and plan and deliver support accordingly. It’s really important for providers to feel that they can sit down and have a discussion and be pragmatic about it.
Commissioners also need to be aware of the impact of their required quality monitoring and compliance processes within a person’s own home. For example, Paul does not always want the senior managers from Aurora Nexus to come into his home and read all of his support records. That is his right. When they are there, he wants to chat and show them what’s happening in his life.
As a provider they know they can find out a lot about what’s happening by being present alongside all the other information they can collect that doesn’t impact on Paul in his home. But the provider still needs to be able to complete some sort of quality audit to satisfy regulatory and contractual requirements, so there is a need to think flexibly about this aspect of monitoring and managing support provision as well. This needs to come both from CCGs and Local Authorities.
As a provider, Aurora-Nexus has received an overall ‘Outstanding’ in its CQC inspection, reflecting its outstanding commitment to outcomes and personalised support for the people it works alongside.
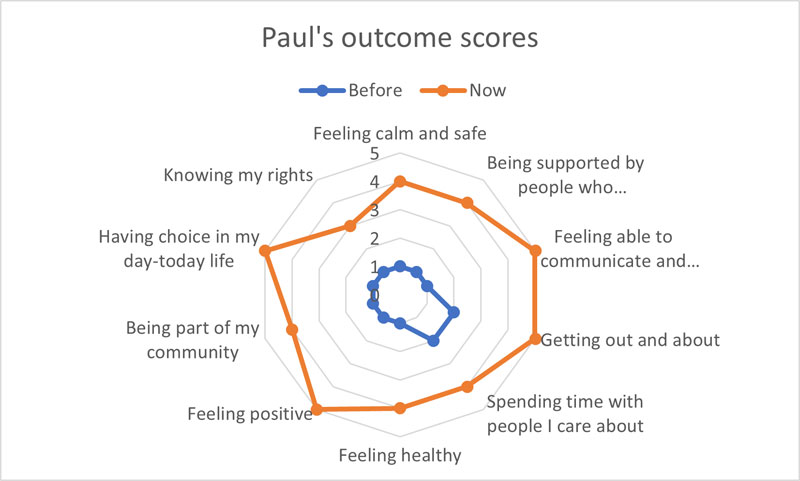
feeling calm and safe 1 before and 4 now.
being supported by people who understand me well 1 before and 4 now.
feeling able to communicate and being listened to 1 before and 5 now.
getting out and about 2 before and 5 now.
spending time with people I care about 2 before and 4 now.
feeling healthy 1 before and 4 now.
feeling positive 1 before and 5 now .
being part of my community 1 before and 4 now.
having choice in my day-to-day life 1 before and 5 now.
knowing my rights 1 before and 3 now.