The right funding, freedom and focus: an approach to improve people’s lives and protect public services.
Introduction
The right funding, freedom and focus: an approach to improve people’s lives and protect public services.
Councils need:
- a relentless focus on prevention and wellbeing to improve population health, reduce health inequalities and help reduce the long-term cost of care and treatment and to maintain sustainable health and social care services
- increased and sustainable levels of funding for adult social care and public health to stabilise the market and help meet current unmet needs
- real freedom for local leadership to focus on what is important for local communities.
A citizen’s right to good health
Every citizen has the right to good health and wellbeing to enable them to make a full and positive contribution to their families, neighbourhoods and wider society. A range of recent polling paints a stark picture of a public that is concerned about current health and care provision and its outlook for the future. [3] Of local government’s many responsibilities, none are more vital than creating places that promote good health and wellbeing.
Councils are uniquely placed to positively influence many of the wider determinants of health, such as housing, education, the environment, economic growth and skills. We work hand in hand with our communities, people with lived experience of services, the NHS, businesses and many other stakeholders to create the conditions necessary for good health. This activity is powered by three key forces:
- public health
- the interface between local government and health
- adult social care and support.
Together, these forces drive forward action to improve and sustain individual and population health and wellbeing.
Too often, councils are driving that approach in spite of national priorities rather than because of them. Funding is a central issue. Whether it is a lack of funding, its late delivery to councils, its often-short-term nature, or stringent accompanying conditions, funding issues can severely curtail the ability of councils to maximise their impact. But it is not just a question of money. The ability of local leaders to lead can be hampered by both national directives that stifle local priority setting and a narrow approach to accountability that only looks upward, rather than outward to communities and citizens. Of equal importance, our model of health and care focuses too much on treating sickness and not enough on preventing or delaying the onset of conditions which require more acute and costly support.
The experience of the pandemic powerfully illustrated how effective local government – working with its statutory and non-statutory partners – can be in supporting the wellbeing of people and communities. We need to build on this experience to usher in a new commitment from government to improve people’s lives and bolster public services.
With such a commitment in place, we will create the optimum conditions for strengthening the resilience of individuals, our communities and our health and care services, and ensuring those services make their full contribution to the economy.
[3] Research (November 2022) by the Health Foundation and Ipsos tracking the public’s views on health and social care
Mission to reality
Focus on prevention and wellbeing
The LGA has consistently argued that the current social care and health system is unsustainable and will buckle under the weight of demand unless we urgently invest to protect health, prevent sickness and intervene early to minimise the need for costly hospital treatment and care.
Focusing on treatment alone is not the answer. We need preventative strategies that mitigate or defer the need for costly interventions and at the same time deliver better outcomes for individuals.
The UK’s health challenges are significant. Rates of smoking remain high among some groups, levels of obesity are among the worst in western Europe and rates of harmful alcohol consumption, which were already high, increased during the pandemic. Around 40 per cent of premature mortality in the UK is caused by preventable conditions such as cardiovascular disease, diabetes and cancer. We know that preventive public health services such as smoking cessation, weight management, health visiting and sexual health services are essential to prevent disease, improve people’s quality of life and reduce health inequalities.
2023 marks the tenth anniversary of the transfer of public health from primary care trusts to local government. The shift was one of the largest ever transfers of funding and responsibilities from the NHS to local government. It allowed public health to embed health and wellbeing across all the council functions that impact on the public’s health. Despite the constrains of reduced funding, it enabled public health to capitalise on councils’ role as place leaders, coordinating partnerships across the NHS and a wide range of other organisations, and with communities, developing the ethos that ‘health is everyone’s business’.
Analysis by the University of York suggests that the expenditure through the public health ring-fenced grant provided to local councils is three to four times as cost-effective in improving health outcomes than if the same money had been spent in the NHS.
Health is more than healthcare
Health is much more than healthcare, more than the NHS. As identified in the reports from Professor Sir Michael Marmot’s Institute of Health Equity, to truly improve the nation’s health and turn around the growing gap in healthy life expectancy, we need to act on the social determinants of health such as poverty, poor housing, poor environments, and worklessness. The role of councils in tackling the root causes of poor health is crucial, particularly given the strong focus on place, wellbeing and cross-sectoral working which social determinants approaches require, and which local government is well set up to deliver.
Prevention Transformation Funding
We have to be candid about some of the financial and budgetary implications of upscaling prevention. A significant proportion of funding is still tied up in treatments. We recognise that providing additional financial support is exceptionally challenging, especially given the financial pressures across the public sector. But without resources specifically for prevention, we won’t see the radical step change required to reduce impacts on the NHS and adult social care. The Government should introduce a Prevention Transformation Fund. This would enable some double running of new investment in preventative services alongside ‘business as usual’ in the current system, until savings can be realised and reinvested into the system. We can learn lessons from other areas such as learning disability where we have already seen a shift from a model of institutional-based care to community-based models of delivery. This achieved system efficiencies and released resources over time, even if an element of ‘double-running’ costs was needed to move from one delivery model to the other.
We can also learn from international examples. In America, the Obama Administration established the ‘Prevention and Public Health Fund’ (PPHF). The PPHF was established as part of the Affordable Care Act of 2010. Established by law, it was the nation’s first mandatory funding stream dedicated to improving the nation’s public health system. The PPHF provides expanded and sustained national investments in prevention and public health, to improve health outcomes, and to enhance health care quality. The Fund invests in a broad range of evidence-based activities including community and clinical prevention initiatives.
An investment in the public’s health
The Government must provide long-term resources to public health, which improves the health of society, advances equity, and fosters economic resilience. It is fiscally sensible to invest in public health to help reduce the long-term cost of treatment and to maintain a sustainable health and social care service.
Good health is vital for prosperity, enabling people to play an active role at work and in their communities. Giving children the best start in life reduces demands on GPs, hospitals and social care. It means children start school ready to learn and to achieve, so our schools can be more effective, and we have an economically active workforce in later years and the best chance of people being safe, happy and healthy throughout their lifetime and into old age.
Good practice shows just what potential there is for public health, if properly resourced, to improve health and wellbeing. Public health teams, working with a ‘health in all policies’ approach, are tackling ongoing health challenges such as obesity, mental illness, alcohol misuse, sexually transmitted infections and the impacts of isolation and loneliness in old age, as well as addressing some of the serious health inequalities that still exist within and between communities.
Funding for adult social care
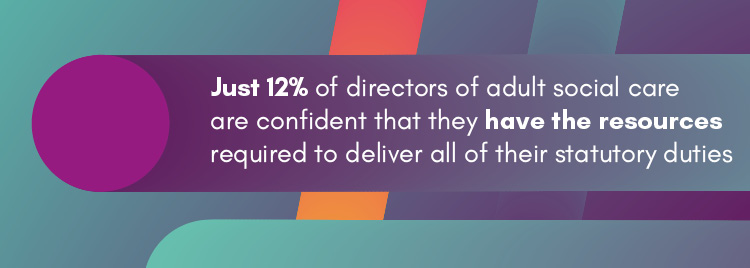
Survey work by ADASS shows that just 12 per cent of directors of adult social care are confident that they have the resources required to deliver all of their statutory duties. The survey also reveals directors’ concerns about growing demand, the position and experience of unpaid carers, the fragility of the provider market, and reductions in quality and choice within local care markets. The difficulty of recruiting and retaining care workers is a major concern shared by many across the sector. Further survey work by ADASS shows that nearly 300,000 people are now waiting for an assessment of their needs. Known pressures will swell costs further, particularly the increase in the National Living Wage (NLW). Combined inflationary and demographic pressures will also require additional funding.
We welcomed the money announced for adult social care in the 2022 Autumn Statement (up to £2.8 billion in 2023/24 and up to £4.7 billion in 2024/25) but much of it will be absorbed by meeting pay and inflationary pressures and it falls short of what is needed to allow councils to fully deliver against their care act responsibilities and to tackle workforce and market pressures. It should also be noted that some of this funding may not be available to fund adult social care:
- The funding for the adult social care discharge grant will be split between councils and health bodies. Consequently, councils will receive £800 million over the next two years from this grant rather than the full £1.6 billion.
- For each of the next two years, social care councils are able to raise their council tax rates by up to 3 per cent without requiring a referendum. They can also raise an adult social precept of up to 2 per cent. The headline adult social care figures announced at the Autumn Statement assume that all social care councils will raise both their council tax and adult social care precept to the maximum. Consequently, the assumed new funding from council tax flexibilities is best seen as a potential maximum amount, rather than as guaranteed new income to support adult social care.
- The social care grant provided to councils will increase by £1.3 billion in 2023/24. However, this grant is for adult social care and children’s social care. The Association of Directors of Adult Social Care Services’ (ADASS) 2022 survey indicates that, on average, councils allocated 41 per cent of their 2022/23 allocation of this grant to children’s social care.
Additional funding is needed to allow councils to fully deliver on the full range of its statutory duties under the Care Act. Performance against the duties under Part One of the legislation is what the Care Quality Commission will assess councils on through the new system of adult social care assurance. The Care Act remains a well-supported piece of legislation, but its full intent has never been realised owing to the funding pressures – particularly social care’s wider preventative duties and the role it plays in supporting discharge and helping people recover from time spent in hospital. A substantial injection is needed to help tackle unmet and under-met need through investment to expand provision and in new models of care for those already receiving support and those who currently do not. We could also invest in housing provision and funding for the voluntary and community sector, which supports people who do not meet eligibility thresholds, as well as supporting wider recovery for people who have spent time in hospital.
Adequate and sustainable funding for adult social care is a necessary but not sufficient condition to bring about the changes we need to ensure everyone who draws on care and support can live their best life. Alongside funding we need a commitment to wider reform that tackles the most important issues. The Government’s recent ‘Next steps to put people at the heart of care’ plan (following on from its December 2021 white paper) constitutes a significant watering down of previous white paper promises which, even as they stood, would only have taken us on the first steps towards a more sustainable and refocussed future for care and support. It is particularly disappointing that investment in measures to support the care workforce have halved from £500 million to £250 million and a planned investment of £300 million for housing transformation has been dropped. There have been a number of recent inquiries and commissions that have pointed towards a brighter future for social care, using the vision put forward by Social Care Future as a starting point:
The Government must work with the sector, and crucially people who use social care services, to expand on their ambition and bring about the changes needed. But this is not a one-way conversation and the sector – in which councils, providers and the community and voluntary sector are already pointing the way forward with countless cases of best practice – should continue making the case to the public about the inherent value of care and support to us all.
Working in partnership with ICSs to improve health and care services
Local councils are vital partners in integrated care systems (ICSs), introduced in 2022 to drive a joined-up approach to health and care services and health outcomes between different NHS organisations and between the NHS and its partners in the wider health and care system. It's only by working together that we can provide person-centred care and support needed for our growing population of people with long-term health conditions. It is also the only way that we can redesign our approach so that we invest more in promoting health and wellbeing to avoid people becoming ill.
The Hewitt Review into the autonomy and accountability of ICSs made far-reaching recommendations on performance management, prioritisation, decision-making and accountability. The review echoed many of the LGA’s messages on local leadership for health and wellbeing.
Freedom for local leaders to lead
Each place is unique in it in terms of its population, the health challenges, the landscape of health, care and wellbeing services and as such, they require the flexibility and freedom to identify their own targets for improving population health outcomes. That said, there is a lot we can, and do, learn from each other through a positive learning culture and sharing good practice.
Let local leaders lead
We recognise that the Government leads the policy agenda and it is appropriate that they should set a small number of strategic priorities for ICSs. But these should be focused on outcomes rather than process or activity. This will give local leaders of ICSs and place-based partnerships, including health and wellbeing boards, the space and flexibility to focus on the priorities that are most important for their communities.
Don’t reinvent the wheel
We are not starting from scratch. Many areas have been working for years and to join up care and support to achieve better services and better outcomes. We need to learn from them and, where they are working, leave them to get on with the job.
Subsidiarity and devolution don’t stop at ICS level
ICSs potentially represent a major devolution of resources and responsibilities for the NHS, moving from a top-down, centrally driven institution to one in which the 42 ICSs are the local leaders. But ICSs also need to devolve power, decision-making and resources to the most local level appropriate. In many cases, this will be the place and neighbourhoods defined by local government places. Local authorities are the natural leaders of place. We already have HWBs responsible for identifying local priorities and agreeing shared strategies for achieving better health and wellbeing outcomes – ICSs need to support and enable them rather than duplicating or bypassing them.
Accountability upwards to NHS England and Government is important but so is accountability outwards to local citizens
For too long there has been a democratic deficit in the NHS. ICSs need to work closely with councils and their elected members to ensure that their integrated care strategies and Joint Forward Plans reflect local needs, concerns and aspirations in a clear set of local ambitions for all partners. Local authority overview and scrutiny also makes a major contribution to ensuring that the NHS is locally accountable.
Promote and embed a learning culture
At all levels. It’s not about telling people what to do or promoting a single approach in all ICSs or places but everyone committing to promoting a learning culture. NHSE and DHSC can support this by promoting a peer-led approach for ICSs, such as the one developed by the LGA to drive improvement in councils. We already co-produce and jointly deliver a peer-led support programme for systems and places in partnership with NHS Confederation and NHS Providers.