Introduction
The last 15 months have been unprecedented. No-one could have imagined they would have to live through times like these. Although we are now finally emerging, the impact of COVID-19 will continue to be felt for years to come. The pandemic has both brought out the best in us and exposed society’s fault lines. Most of all, it has given us a new perspective on longstanding issues, which we will need to address if we are to rebuild our communities.
The Government’s national strategy to tackle the pandemic coordinated the effort to protect jobs and businesses, roll-out vaccinations and provide information to the public. But it is local government, as its delivery partner, that has turned this response into a reality on the ground – local responses recognising different local needs and impacts across all of the country’s diverse communities.
The immense value of the strong local leadership provided by councils and the exceptional commitment of councillors and council staff, who have been on the frontline in the battle against the virus, cannot be understated. They are among the true heroes of the pandemic and, working closely with central government, local NHS partners, voluntary and community groups, have put in a monumental effort to support and protect local communities.
Central and local government have shown what can be achieved during a crisis when we work together towards a shared goal. Tens of thousands of rough sleepers and homeless people helped off the streets; millions of the most vulnerable shielded from the virus; and billions in vital grants provided to businesses forced to close. Councils, with their directors of public health, have also been at the centre of efforts to limit the spread of COVID-19 in all its variants and support our hugely successful vaccination programme. Local government can be, and has been, trusted to deliver on national priorities.
COVID-19 has brought about rapid societal change, transforming people’s attitudes, behaviour and aspirations. People are working differently, shopping differently and socialising differently. For many people their local area matters more now than it ever did and it will continue to play a significant role as we move out of the pandemic. Some groups and communities have been particularly affected by the health, social and economic impacts of the pandemic and will need more help to recover. Whilst for some, the issues they faced pre-pandemic – access to fast broadband, housing that is right for them and their families – have been amplified. This means that the role councils play will have a greater significance in the lives of people as we all reimagine what our post-pandemic lives look like.
There is an opportunity here, for us all to work together to retain that concentrated focus on our local communities. And it must be local: there is no single solution that will work in every place. Whether it’s microbusinesses or an anchor employer; pockets of deprivation; older people or a yearly influx of students; a thriving cultural scene: every community has unique strengths and challenges.
Councils want to build on this momentum and work with Government as equal partners to achieve our shared ambition to level up communities that feel left behind by investing in people and transforming places across all parts of the country.
One of the most important lessons from the COVID-19 crisis is that public services are at their best when Government enables councils to innovate and create new services locally. Throughout the pandemic councils have shown that they can move swiftly to adapt local services to meet national objectives in the context of local needs. Overnight, shielding services were created to protect the vulnerable. Councils have also assisted test and trace activity and carried out targeted work with vaccine hesitant communities. In all these cases councils have built services which meet the needs of their specific communities.
We need to value difference and the local voice. Understanding local difference enables the delivery of services which genuinely level up communities. Local differences should be seen as responding to local need and making the right interventions for that place.
That is a mark of strong and responsive leadership.
In this paper we will explore a series of ‘pen portraits’ to give a resident-centred view of local services and explore the future journeys our residents will be taking. They are imagined reflections based on the experiences of people across the country. They demonstrate that, as we look to build back better from the devastating social and economic impact of the pandemic, our communities will need councils and the local services they provide more than ever. As the pen portraits show, our children, our local business owners, those looking for work or to upskill, our neighbours, family, and friends all use and rely on council services on a daily basis. If we’re truly to come out of this pandemic with a society that’s levelled up and that works for all, councils’ work will be at the heart of it.
We also look at a range of ways that our sector support programme, funded by Government, has supported councils in responding to issues triggered by the pandemic, including challenges relating to recovery and renewal.
More often than not, when the Government sets an ambitious target or new policy ambition, it is councils they need in order to deliver it. It is clear that if the Government is to fulfil its pledge to level up the entire country and improve the lives of its citizens – every single person, every single family – it cannot succeed without adequately funded and empowered councils.
Levelling up cannot just be a political slogan. It has to mean a radical reset of the relationship between central and local that leads to real change for people’s lives. This paper set outs why now is the time for Government to broaden its thinking and explores what success could look like for communities.
Over the last decade, England and Wales have taken some steps to give greater freedom to local communities. The COVID-19 crisis has proved that we need to go much further and much faster. Bringing power and resources closer to all of us is the key for all our communities to thrive, level up the stark inequalities the pandemic has exposed, develop a green recovery, address the skills gaps and revive the economy so that it benefits everyone.
This is a vision supported by many in Parliament and by residents. Local Government Association (LGA) polling shows more than three quarters (77 per cent) of MPs say local councils are best placed to administer the delivery of public health and 72 per cent believe they are best placed to run contact tracing to manage the spread of COVID-19. It also shows that eight in 10 MPs (80 per cent) say councils should have more financial freedoms and powers to build homes in their area and almost three quarters (72 per cent) say they should have more control over local taxes.
Our own polling also shows that three quarters of people trust their local council to make decisions about how services are provided in their local area.
Investment in local services is also vital to our national economic and social recovery and to ensure councils can continue to make a positive difference to their residents’ lives, help reduce pressures on the rest of the public sector and save money for the public purse.
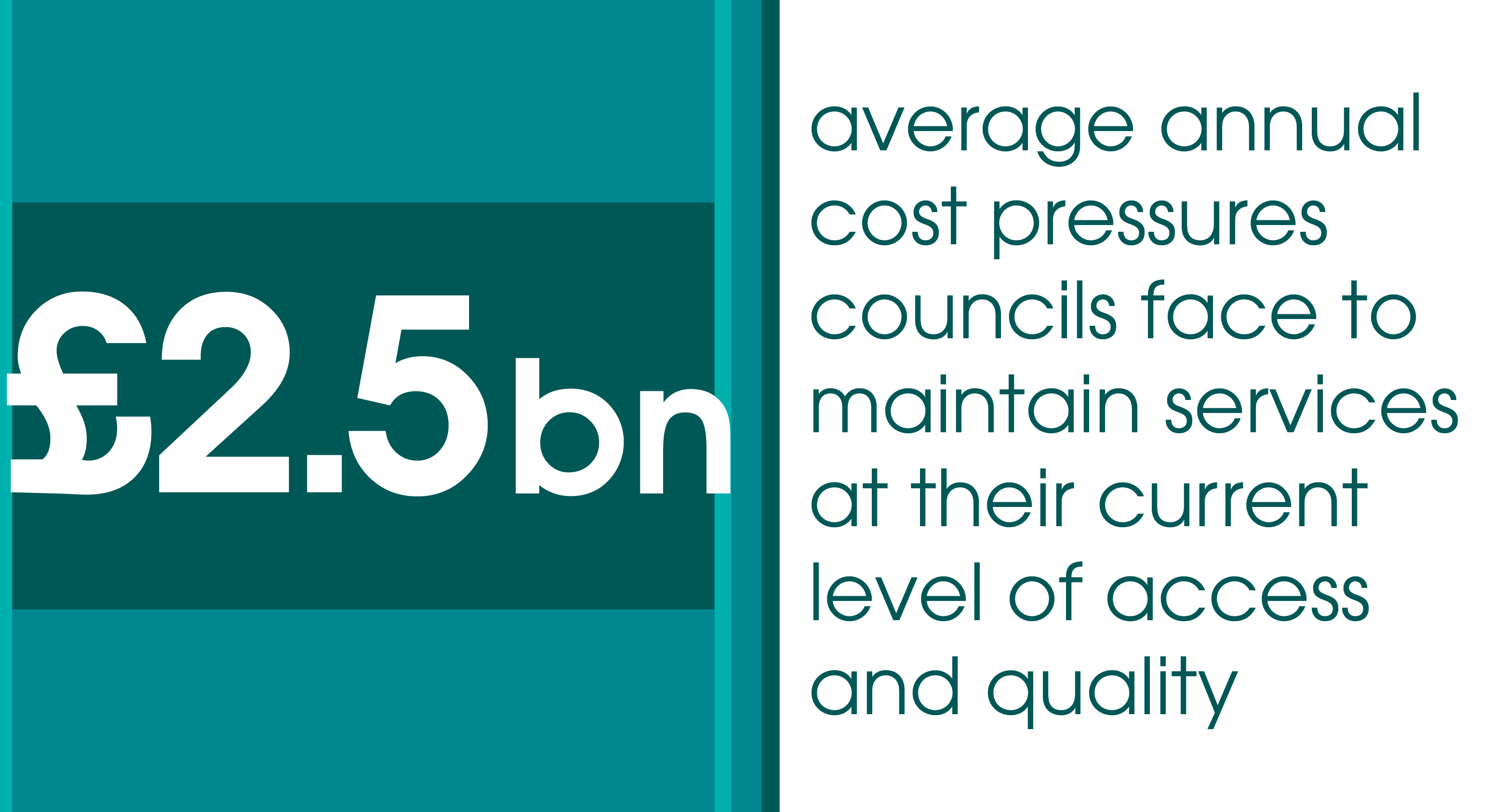
As our pen portraits show, very often it is those who are most vulnerable and need support across a range of services to improve their life chances, that rely on our local services the most. Demand pressures continue in children’s services, adult social care, and efforts to tackle homelessness. Early LGA analysis ahead of the forthcoming Spending Review shows that councils face average annual cost pressures of £2.5 billion to maintain services at their current level of access and quality. Of this, £1.1 billion per year is related to adult social care (in addition to the £1.4 billion provider market pressure), £0.5 billion to children’s social care and £0.9 billion to all other council services (excluding education). This does not take into account any continued impact of the pandemic, for example catching up on pent up demand in children’s social care or longer-term effects on sales, fees and charges or commercial income, especially impacting culture, leisure and sport services.
Local government is efficient and focussed on managing taxpayers’ money effectively. If the forthcoming Spending Review facilitates a multi-year settlement that puts local government funding on a long-term sustainable footing. This would enable councils to more efficiently plan local services, so vital during the pandemic, and help reduce demand and cost pressures on other parts of the public sector.
With the right funding and freedoms, councils can help Government achieve its ambitions for our national recovery from the pandemic, drive improvements in public health, boost local economic growth, revive town and city centres, build more homes, improve our roads, improve the life chances of children and young people, support older and disabled people to live well and equip people with the skills they need to succeed so no one is left behind.
Local government is part of the fabric of our country. It has demonstrated its ability to lead on the most pressing issues facing our communities, right across the nation. Using local leadership is the only way we will be able to tackle the significant challenges that lie ahead and ensure we improve lives and build growth for all. That is a powerful offer to Government and a proven route during this pandemic that should now be the cornerstone of our national recovery.
As we come through the most difficult period many of us have ever faced, our communities cannot afford us to miss this vital opportunity to build back local.
Children and young people
This pen portrait is an imagined experience, based on the interaction between residents and councils and councillors across the country.
Lucas, 11, lives at home with his parents and his eight year old brother
When there was the virus loads of kids didn’t go to school which was really weird. I still went which was good because I like lessons, but I didn’t get to see some of my friends for ages. Because our lessons all got messed up, I have a tutor now to help with maths. She’s really cool and makes it fun.When we had lockdowns, my social worker couldn’t come to our house but he called me on Zoom which I liked better, and we went for some walks in the park which was good. I’m not sure what will happen now, but I hope we can still do the Zoom calls.
I really hope things are more normal now. I’ve started doing football lessons and we’re going swimming again. My brother is autistic and swimming makes him feel better so it was hard when we couldn’t go.
I’m going to secondary school soon – I’ll have to get a bus there which is a bit scary, but the school has a really cool science lab where you do real experiments so I’m excited about that. I want to be a scientist when I’m older! I’m really glad I didn’t have to change schools last year. My friend Jack in the year above didn’t even get to say bye to his friends or have a leaving party or anything. He was really sad and didn’t even want to come to the park for a while.
Delivering during COVID
Children made enormous sacrifices during the pandemic, experiencing huge disruption to their education and losing out on time with their friends and wider family. For teenagers, those sacrifices saw many miss out on their exams, jobs and traditional rites of passage. Our young people will feel the impacts of the pandemic for many years to come.
Councils played a vital role in keeping children like Lucas safe and supported during the pandemic, pivoting quickly to find new ways to deliver services and to keep the most vulnerable children safe. They worked closely with schools to keep them open for vulnerable children and children of key workers, tackle COVID-19 outbreaks and interpret Department for Education (DfE) guidance. When schools closed to most pupils and some children risked being lost from view, children’s social care departments worked with schools to put in place plans to keep them safe, including continuing face-to-face visits even when most in-person work shut down. The relationship between councils, early years settings and schools proved vital through the pandemic, not only in keeping children safe but keeping their education going and supporting public health efforts.
Support for families was moved online wherever possible to keep relationships going, while councils found new ways to make sure children in care could keep in touch with their birth parents and siblings, from video calls to online games. And care leavers were able to stay with their foster carers or in their children’s homes for longer, rather than moving into independent accommodation in the middle of a pandemic.
Councils and schools rallied round families to provide as much support as possible, working in partnership with government to distribute millions of pounds of funding to support those in need, from food parcels and vouchers, to help with fuel costs, IT equipment to help vulnerable children learn online, adapting schemes as the pandemic evolved to make sure local families got what they needed. Councils also organised holiday activities and kept parks open wherever possible to give children vital opportunities to play – especially important for those children living in homes without outdoor space.
How can we make sure that all children thrive and are given bright futures?
Wrapping services around children in a myriad of ways must be the approach we take to building a child centred recovery. Councils understand their communities and are perfectly placed to make sure children like Lucas and their families get the joined-up support they need, both through the hundreds of services they deliver and by working with government and local partners. The pandemic demonstrated the power of strong relationships between government, councils, and schools. We need to recognise the value of these relationships and what more they could offer in the future. To do this we need to collectively work on some fundamental issues:
- Invest in preventative and early help services
As the wider and longer-term impacts of the pandemic become apparent, it will be more important than ever to make sure the right services are there to help families like Lucas’s through difficult periods. There is a real opportunity here for the Government to invest in preventative universal and early help services – via councils and the NHS – so that children, young people and their families can get the support they need, as soon as they need it, and before problems escalate. This would particularly help with issues such as children’s mental health and local safety nets which can help families to avoid a crisis when finances are tight, keeping them in their homes for long enough to get back on their feet. Preventative services can ensure children and their families get enough support to get through a tough time while building the resilience that will help them cope with future challenges. Investing in the very early years is particularly important and we know that integrated working between partners, alongside a clear offer to families can make a real difference to children and their families.
- A cross-Whitehall strategy putting children and young people at the heart of recovery
As leaders of their place, councils bring together schools, partners and their services – including housing, public health and transport – to improve children’s lives and help them make successful transitions to adulthood. The cross-service and cross-sector work exemplified at a local level needs to be replicated nationally. Greater join up across government departments could help to improve outcomes for families. For example, better data sharing across government departments would help us to ensure that more disadvantaged and disabled children are accessing their full early education entitlements. It would mean that initiatives, such as integrated care systems, deliver better outcomes for children. And it would help us look at how we make sure children are growing up in good quality homes close to good schools, their family and friends. Local government would welcome the opportunity to work with central government to develop a cross-Whitehall strategy which focusses on how we can level up for the next generation.
- Reform the Special Educational Needs and Disabilities (SEND) system and recognise council’s role in education
There is an unprecedented demand for additional SEND support for children in our schools driven by a rise in the number of children with complex needs and raised parental expectations. The most recent reforms in 2014 also allowed for greater choice for families without funding councils to be able to meet the need.
The current SEND review is an ideal opportunity to make sure that the system is working for children and young people. A reformed SEND system, which prioritises mainstream inclusion and a reduction in the use of expensive independent non-maintained special schools will provide some relief for hard-pressed council high needs funding blocks.
The 430,000 children and young people who already have an education and health care plan (EHCP) will continue to be entitled to the support set out in their plans up to the age of 25, meaning that these costs are ‘baked in’ for councils and partners. The DfE will need to ensure sufficient high needs funding is made available to support these children and young people as they work their way through the system. In a reformed SEND system EHCPs must focus on helping children and young people achieve the best possible outcomes and live independent lives as they move into adulthood. As children and young people grow and develop the SEND system should also allow for the support set out in EHCPs to be ‘stepped down’ and plans removed if they are no longer required.
We want to work with DfE to ensure that councils can continue to play a positive role in supporting schools. Councils have a proven track record in driving up school standards and creating new school places. Where schools are failing it is vital that improvement support is provided quickly to ensure that the impact on pupils is minimised. Maintained schools should be allowed to sponsor failing academies without having to become academies themselves.
To ensure there’s a school place for every child the existing highly fragmented school capital funding system should be replaced with a single local funding pot, bringing together existing programmes to create additional places and rebuild, maintain and repair schools. Councils should also be allowed to open new maintained schools where that is the local preference and be given the same powers to direct free schools and academies to expand, as they currently hold for maintained schools. - Working towards a more sustainable funding base
Together, councils and government can change the lives of millions of children for the better. To do this we have to have an honest and open dialogue around the funding issues within the system. Prior to the pandemic these services were already tackling financial challenges. The current system is increasingly focussed on the most urgent cases. Child protection work is increasing and historically many children’s services departments have had to cut back early help services which can prevent children, young people and families from needing more costly support later on.
Reviews of the SEND and children’s social care systems will help to consider both the funding challenges and how these systems work for children and families, from where children with SEND can best access their education, to addressing the spiralling costs of homes for children in care which may not fully meet their needs. But there will remain a need for a broader dialogue about how we achieve the ambition of a child centred recovery and how this can be funded. The Spending Review provides a perfect opportunity to create a more sustainable funding position for children’s services. A position which reflects the investment which will be needed to support children through the future phases of their lives.
If we build back local, we can support children, like Lucas, and their families with a range of services that help to deliver a brighter future.
The pandemic has shown us that collectively schools, councils and national government can work at pace to deliver the range of support children and young people need to thrive. The inequalities highlighted during the pandemic must make us redouble our focus on narrowing the gap in achievement between the most disadvantaged children and their peers, and the importance of harnessing the powers and resources of all local public services to deliver this.
When we look back on the pandemic, we should remember that the strengthened relationship between schools, councils and government kept children safe, schools and early years settings open for the most vulnerable, and highlighted the importance of supporting children to thrive in all aspects of their lives. The children’s workforce was instrumental to this. It is the strength of these relationships and this workforce which we now need to build on to deliver the levelling up our children and young people deserve.
Children and young people: sector support at a glance
Children’s improvement advisers have continued to provide intensive support, guidance and challenge to councils to help shape support for vulnerable children throughout the pandemic, while peer challenges and diagnostics have been refocussed and delivered remotely in 17 councils. Key themes of focus have included children’s social care, SEND, school improvement, early years and youth justice. Also, delivered remotely, our programme of early years virtual learning and support, involving an intensive programme of webinars and action learning sets has had over 3000 participants.
Public health
This pen portrait is an imagined experience, based on the interaction between residents and councils and councillors across the country.
Mary, 57, and Keith, 59 are a married couple and live together
The past year or so has been a bit of a struggle. Keith and I always kept ourselves to ourselves. When COVID first came in March I was really scared. Keith used to laugh at me. But I was worried because I’m the main carer for my 85-year-old mum who lives near us on the estate. I wasn’t sure if I’d be allowed to carry on seeing her. I do everything for her. Her shopping, her cooking – and she likes the company. But the council was really good. Someone phoned my mum and offered to send her a food parcel and checked to see if she needed any other help. In the end we didn’t need it as I just did everything for her. But it was nice to know that the housing officer knew that mum was alone and might need help.Then things seemed to get better and we even went out in the summer, but then in the early part of 2021 we both got COVID pretty nastily. The doctor said that in the future we need to think about quitting smoking and getting fitter. I was worried about my mum as I couldn’t go and see her. I got in touch with the council again and they were really helpful. Firstly, they said we qualified for test and trace self-isolation payments. Secondly, they got mum some help with her shopping and arranged for her medicines to be sent directly to her home.
After having COVID I decided I wanted to get my vaccination done as soon as possible. Keith wouldn’t go, said he wasn’t going to be told to have a jab. I got really upset and spoke to the doctor. Then this community champion man came to our house. He had a long chat with Keith and left these leaflets. In the end Keith came round and decided to get his vaccinations done.
We are all vaccinated now. But I’ve been thinking about what the doctor said about us stopping smoking and getting fitter. It’s just all really hard to do at our age and we can’t afford any of those expensive slimming programmes or ‘quit smoking’ courses. I’m hoping this local ‘healthy lifestyle service’ that the GP mentioned will be able to offer me and Keith some help.
Delivering during COVID
Throughout the pandemic public health services commissioned by local councils have worked quickly, efficiently, and creatively. Public health has used its experience in communications, behavioural insight and health campaigns to engage with local people to tackle outbreaks and maintain safety. Councils have been flexible and innovative in keeping health and wellbeing services running through digital options and has sought to tackle the impact of the pandemic on health inequalities.
Significant work has been undertaken to establish mechanisms for supporting vulnerable people during the pandemic. This work cuts across a number of key stakeholders from local government to the NHS, local resilience forums (LRFs), food distributors, food charities and the wider VCS. This work meant that collectively millions of vulnerable people – like Mary’s mother, were shielded and received food and medicine parcels, additional support was provided for surge testing and outbreak management, special programmes were delivered to increase the uptake of the vaccine in difficult to reach communities and other essential public health services, such as sexual health and mental health support, moved online so that people still got the help they needed.
Public health in local government is at the heart of local work to tackle the virus. It provides the leadership, expertise, partnership-working and access to local resources that are fundamental to the strong place-based coordination of health protection and health improvement.
From a local perspective, getting the right balance between national and local measures to tackle the pandemic has been an ongoing challenge. There is appreciation for the hugely difficult job national government had in responding to the pandemic, and an understanding that some measures are most effective when coordinated and delivered on a national basis. Not least of these was the vital national decision to prioritise the development, purchase and speedy roll-out of vaccinations.
However, throughout the pandemic, council leaders have called for greater involvement in decision-making and better dialogue before national announcements about measures with implications for local areas. Moving forward, it is essential that there is greater recognition that public health, wider local government, and local partners have the skills, expertise, local knowledge and infrastructure to play a major role in combatting local outbreaks.
Directors of public health feel personally responsible for protecting the health of people in their areas and need the tools to do this well. Two key areas of concern were restricted access to nationally collected data and an initial lack of local involvement in contact tracing. As a result of shared experience and learning between national and local organisations there have been improvements throughout the year, but this took time.
Moving forward, public health cannot be in a position where it faces restricted access to nationally collected data, particularly information about the locations of people testing positive at postcode level, as this hampers the ability of the service to monitor, analyse, model and take action on local virus patterns and outbreaks.
There is a strong view in local government and public health that if sufficient data had been shared more quickly then contact tracing could have been localised sooner. This would have led to a more affordable, swift and effective system. For this to work, a ‘team of teams’ approach is needed with the responsibilities of each part of the system clearly articulated and properly resourced.
Research is taking place into the effects of people experiencing long COVID symptoms. Less is known about the longer-term impact of living through the pandemic on the general public – their mental wellbeing and resilience, for instance – more information will emerge in time. The pandemic has had a major impact on the health and wellbeing of our society and recovery will be a priority for public health for many years.
As we come to live with COVID, services will need to be on constant high alert, to be responsive to new variants of concern and act swiftly to get on top of areas with enduring transmission.
Public health teams in councils have been at the forefront of this tremendous local response to the pandemic and are ready to work closely with the new UK Health Security Agency (UKHSA) and the Office for Health Promotion. It is more than evident that responding to and recovering from an outbreak of this scale should start at the local level, working closely with national agencies.
The UKHSA needs to be able to operate nationally as a global player to major health threats. This should then be aligned with councils’ ability to react swiftly on the ground, using their local knowledge, expertise and skills. It is vitally important that we clearly define the role and accountability of each, as well as devolve more leadership, control and resources to councils. Health inequalities between the most and least deprived have been exacerbated by the pandemic, so it is essential that any future model for health protection be intrinsically linked with health improvement, if we are to realise real improvements for our residents.
It is widely accepted that prevention is better than cure. The Office for Health Promotion has an opportunity to enhance this focus on prevention. All parts of the public health system – including councils’ public health services – have a role to play in promoting healthier choices, preventing sickness and intervening early, to reduce the need for costly hospital treatment and social care. By embedding prevention as a core focus of its strategy, the Office for Health Promotion will ensure the best outcomes are achieved for people.
How can we empower local public health to improve the health and wellbeing of local communities?
The Government’s levelling-up agenda was important before the pandemic and is now even more essential for a stable and prosperous future. A comprehensive, ambitious and energetic drive to tackle the social determinants of health at national, regional and system level must take place and be properly funded.
Local government and public health should work with national and system partners to develop a new model for health protection – one which does not just tackle outbreaks or incidents, but responds to the impact on individuals, and harnesses the power of communities.
A full evaluation of the pandemic response is needed, but early suggestions from local public health is that there should be a shift to emphasising the impact on individuals and communities affected. A key example is the issue of people on low incomes with unstable employment finding it difficult to self-isolate for financial reasons, and the Government’s provision of £500 funding to support isolation. The role of voluntary and community organisations in the pandemic also suggests a greater role for that sector in emergency response.
Using online and digital communication has been the cornerstone of making services more flexible. Many were already increasing their digital offers with new contracts for services like sexual health and stop smoking. Some, not traditionally associated with digital communication, like health visiting and drug and alcohol support groups, have developed online offers, which are being evaluated for effectiveness.
While digital communication will never replace one-to-one contact or groupwork, it can be highly effective, provides good value for money, and is popular with many participants who find it more convenient, more relaxing at home, and more environmentally sound.
There are big questions over the longer-term impact on the general population that need to be better understood – for example, will there be longer-term impacts on the mental health of young people, on drinking patterns, on obesity? Public health will be working on these issues in the coming years.
The health, wellbeing and prospects of children and young people, particularly in deprived areas, have been damaged in the pandemic. Early years support forms the basis for future healthy lives, but important services with proven effectiveness, such as support for the first years in life, have often been the victim of economic austerity. Redeploying updated models of support, with enhanced digital offers and a focus on community assets, peer support and positive mental health in families, should be a priority.
At various stages in the pandemic there have been opportunities for local areas to be involved in national/local partnerships to trial new initiatives. Local government is ideally placed to do this because of its reach across infrastructure and communities, while partnerships between public health and academic institutions provides a good basis to pilot and evaluate new measures.
During the pandemic, many councils have reported issues with the availability of sufficiently qualified staff, leading to high levels of service disruption. With a fully funded and resourced workforce, councils can do much more to deliver public health services.
The public’s increased understanding of, and personal involvement in, health, and the upswell of community support during the pandemic are important opportunities which public health can capitalise on when the pandemic recedes. Models previously developed by public health, such as health champions, making every contact count (MECC) and asset-based community development have proved their worth. All of this provides a window of opportunity for the future.
If we build back local now, we can give people like Mary and Keith the support they need to be healthier, safer and happier.
Local areas need to be given the tools and support to understand and address the economic, social and psychological impacts of the pandemic, and the serious health inequalities that have been highlighted and deepened. If this can happen we can start to build an approach which finally addresses deep rooted issues and has a chance of delivering genuine levelling up across the country.
Public health: sector support at a glance
The COVID-19 Response and Coordination programme supported councils with local contact tracing, community testing, surge testing, shielding and the clinically extremely vulnerable (CEV). In collaboration with the Ministry of Housing, Communities and Local Government’s (MHCLG) National Vaccine Deployment Group, we also developed a think piece to support councils in using behavioural insights techniques to encourage greater vaccine take up. Cross-body working has remained an ongoing feature of this work, with coordination between government, council leaders and chief executives, and councils to prepare for and manage outbreak planning in support of local communities.
The Test, Trace and Outbreak Management programme created further tools and resources to address and share leadership challenges, including dedicated sessions and top tips for chief executives and leaders – as well as the establishment of a Local Outbreak Control Plans Advisory Board, which brought together expertise from across local government to support councils to manage outbreaks more effectively.
Jobs, skills, training and welfare support
This pen portrait is an imagined experience, based on the interaction between residents and councils and councillors across the country.
Sita, 36, lives with her husband Jermaine, 33, and their three children aged three, five and eight
I’ve worked at the airport for more than 15 years now, so it came as a real shock when I was made redundant during the pandemic. We were both really worried about how we would cope as a family, especially when Jermaine was placed on furlough from his catering job, and each month was becoming a real struggle to make ends meet.I wasn’t getting anywhere with the job search online and I started to really worry I was running out of options. Plus, I was getting more and more worried about money and that was making it hard to concentrate on the job search. We managed not to get behind with the rent, but it wasn’t leaving much for food or other bills.
I called my council as I was worried about being able to pay my council tax. The lady arranged for us to have a payment holiday and put me in touch with a welfare rights adviser because I’d never been out of work before and wasn’t really sure what I could get. He gave us some vouchers to help with the kids’ food and told me there was other financial advice I could get from them if I needed it. We’ve really looked at our outgoings and the welfare guy helped us to reduce some of our bills. I’ve even managed to start saving a little bit again with our local credit union.
He also suggested I called the council’s employment and skills hub in case they could help with my work situation. They were working with the NHS to get more local people into entry level NHS roles. I wasn’t sure I had the right skills, but they helped me apply for an online introductory course and it turns out a lot of my customer care skills are transferable.
I was really pleased when I got the job. It’s not quite where I thought I would be, but I’ve got to know the team here and I think I can see myself staying on. It did help that the adult learning team from the council stayed in touch, and we’ve even discussed joining a specialist course in the evenings, to help me take the next step. I’m starting to feel more confident about what the future has to bring.
Delivering during COVID
Throughout the pandemic and successive lockdowns, local councils, as leaders of place and conveners of partners, have coordinated employment, training, and business support around their local ‘places’.
Councils delivered over £19 billion worth of grants to ensure local businesses did not go under. Many set up redundancy and recovery taskforces. They helped the unemployed while job centres dealt with universal credit claims, spotted skills gaps in high demand jobs, and sought to fill them, delivered a hardship fund to the most vulnerable, kept adults learning and engaged through community provision– moving it online, and supported local further education (FE) providers.
Alongside this they were instrumental in making a success of the Government’s Kickstart scheme by creating new work placement opportunities – within their own councils and working with local employers – for young people hard-hit by the pandemic. They even set up ‘gateways’, taking on all the back-office issues so that employers and young people could focus on getting the most out of the placement. This made a fundamental difference to the uptake of Kickstart.
The pandemic exposed gaps in both the national benefits system and the local safety net, and showed how much more vulnerable some places and communities were to detrimental impacts. Both Government and councils moved quickly to put in place a wide range of financial, in-kind and pastoral support for households at risk of hardship or concerns about their finances. The swift amendments to the national benefits system – the restoration of the Local Housing Allowance rate and the £20 per week uplift in Universal Credit – were both necessary and welcome. Councils and local partners led the implementation of a wide range of food and financial advice and support to other struggling households, as well as integrating their health and social care support with the emerging national approach. They recognised locally the vital importance of continuing to fund these services alongside the wider benefits system and employment support.
Local government has shown extraordinary capability to lead our communities through the crisis and demonstrated that they are the default natural partners of central government, helping to deliver and coordinate interventions on the ground. They have demonstrated that local leadership is essential in bringing partners, funding, and programmes together to deliver effective outcomes around place. All of this has been done quickly, quietly, and with limited resources by reorientating their employment and skills services.
As the vaccination roll-out continues and the economy opens up, local government is into recovery mode. Jobs and training will once again take centre stage. How quickly areas recover can be influenced by a combination of policy responses: to rising unemployment as furlough ends; businesses’ ability to stay afloat and recruit again; identifying and investing in sectors that have the potential to create quality, new jobs in the short and longer term, including green jobs; retraining people like Sita to find new jobs sometimes in new sectors; and having decent local careers advice and guidance to help make transitions. Bringing all these policy solutions together around place is critical, to deliver meaningful levelling up.
How can we help unlock local potential and deliver greater opportunity in local communities?
Although there are significant challenges ahead, a joint endeavour between local and national government will deliver greater opportunities and the recovery that our local communities deserve. It is good news that the Government agrees, that to level up it will now look to create new jobs and training opportunities across all places so that people don’t have to move to find work.
People want more opportunities, more jobs, progress in careers and good work, locally. To make this happen we need a renewed partnership with central government focussed on:
- The co-design of jobs and skills recovery
Even before the pandemic hit, the employment and skills system was confusing for learners, jobseekers, and businesses. At our last count in 2017, £10.5 billion was spent across 20 employment and skills funding streams managed by eight departments or agencies. Fast forward to today, the Government has rightly introduced vital additional support, including the ‘Plan for Jobs’. It is now more crucial than ever that all of these funding streams (national and local, existing and new) are better coordinated, so the employment and skills offer is simple and clear.
Councils can make this work. They bring a wealth of expertise, and capability to the table and we believe there is much to be gained by national and local government combining resources and expertise to deliver for people and businesses hard hit by the crisis. And they know their communities and so are able to target specific groups – such as young people not in education, employment or training (NEETs) or older jobseekers – more effectively, adapting provision and forging partnerships. With adequate resourcing and powers, and an opportunity to work in partnership at the earliest stage to shape new or re-design existing Plan for Jobs initiatives, including Kickstart and Restart, we will help land well-intended but often disconnected national schemes, so they become greater than the sum of their parts.
- Councils coordinating skills provision locally
The pandemic has shown that we need our local economies to be able to respond quickly to any sort of challenge in the future. Dynamic local leadership enables councils to hold intelligence about the local jobs market and develop the sorts of partnerships which can be quickly brought together to support national initiatives and deliver the economy of the future.
Our evidence has shown that councils’ employment, skills and regeneration teams rapidly responded to the pandemic, added real value to coordinating different provision on the ground and were critical to partnership working. The pandemic has shown how important it is to get the employment and skills offer right for our communities and why partnership matters, to help people like Sita and so many others. Their role must be cemented in the employment and skills ecology
- Work Local/levelling up white paper
Moving beyond recovery and looking ahead to the levelling up white paper later this year, an opportunity to rethink the current top-down approach, our Work Local principles should form a blueprint for skills and employment devolution that works for all people and places. Opportunities to put this into practice include the Shared Prosperity Fund, National Skills Fund, Levelling Up Fund, and forthcoming Spending Review, to start putting this vision into practice. With enhanced powers and appropriate funding, local leaders would be empowered to bring government departments and agencies together to deliver locally determined skills and employment systems, that deliver integrated, targeted support with sustained outcomes.
For a medium-sized combined authority each year, our Work Local model could lead to an additional 8,500 people leaving benefits and 5,700 people increasing their qualification levels, with additional local fiscal benefits of £280 million per year and £420 million to the economy.
- Support for low income and economically vulnerable households
Economic and employment projections suggest that many households will require longer-term support and advice to remain resilient and adapt to a changed socioeconomic landscape. There is an opportunity now for Government to work with councils, alongside the Department for Work and Pensions (DWP), to give greater scope for developing innovative council-led approaches to improving financial inclusion and wellbeing. Crucially, this is not just about short-term emergency support, but about promoting financial resilience and wellbeing in the longer-term. Sustainable, separately identified local welfare funding will enable councils to maintain effective partnerships and referral pathways and offer integrated support that recognises the important relationships between financial capability and wellbeing and other key issues such as homelessness, family conflict and mental and physical health. Councils have demonstrated that this both saves money and improves outcomes elsewhere in the system.
If we build back local now we can create jobs, build resilience and opportunities for people – just like Jermaine and Sita – in all places and deliver a recovery that works for everyone.
If national government works in partnership with councils we can help to level up, ensuring support is quick, targeted and financially effective. We’ll increase the impact of national schemes, help people to find jobs locally and save money in the process.
Jobs, skills, training and welfare support: sector support at a glance
Councils have drawn on our workforce support to increase local skills and capacity throughout the pandemic. Our apprenticeship programme supported over 60 councils, helping them to improve the way apprenticeships were managed and supported during the pandemic. The programme helped to create new apprenticeships, make better use of the levy through transfers to other local employers, and sustain the LG 500+ Apprenticeship network to share and learn at this challenging time.
Return to Work programmes supported councils by responding to specific skills shortages, attracting nearly 70 councils requiring the skills and experience of returners in areas including social work, legal, ICT and planning.
We have helped to provide opportunities for, and access to, social workers through our Return to Social Work programme, helping to restore participants’ practice with Social Work England and providing interested councils access to a pool of more than 300 newly skilled and experienced social workers.
Further capacity was added with programmes to identify qualified professionals to fill specific and/or urgent skills gaps in environmental health and social work. The Environmental Health Together platform drew 224 environmental health officers and had 122 council subscribers; while Social Work Together had 108 councils subscribed and over 1,000 qualified social workers registered.
Economic recovery
This pen portrait is an imagined experience, based on the interaction between residents and councils and councillors across the country.
Florence, 43, is a local businessperson who owns her own nail salon
I started my business a few years ago. I always thought there was a gap in the market locally. I’d been doing home visits but always wanted to open a shop somewhere eventually. A couple of years ago there was this business fair run by the council at our local shopping centre. They were talking about helping people start new businesses. I guess it all took off from there.The council set me up with a small business adviser. This was so helpful. He told me about an event where the council was going to host some pop-ups. I got involved in this and ran my own pop-up. It was a huge success.
I did this for nearly 18 months and started to develop a set of loyal customers. I wanted to take the next step and try to open my own salon, but I didn’t know what it really entailed. So, I went back to the council for some more advice. My adviser suggested that I needed to understand more about health and safety and qualifications and signposted me to the local Growth Hub. Through their website I was able to find some suitable courses.
The council then announced this regeneration scheme for the town centre. They wanted to create a cultural quarter as a lot of the shops were sitting empty. As part of this I was able to get help with finding a small venue to open the shop on a temporary basis. I opened up with a couple of staff and things started out really well.
Unfortunately, COVID hit and then we had to close down. It’s been really tough, but the council has helped me to renegotiate my rent. I was also able to get my staff furloughed. What happens next about recovery really matters for me. I’m not a big chain so I need support which can be accessed by businesses like mine. The advice and support that is out there can sometimes be confusing. I hope the Government understands that. We local businesses are what can make or break a high street. But we need help too.
Delivering during COVID
Councils have always played an important role in shaping local economies and in helping people like Florence. They understand that each place needs a tailored approach which responds to regional variations whilst maximising national support. When the pandemic hit, the sector was at the forefront of supporting the Government’s national package of measures for businesses. Councils paid out over £19 billion in business grants. They were quick to work with their local businesses to ensure that places could reopen in a safe and manageable manner. Throughout the various lockdowns councils provided support and advice to local businesses via a range of phone and online options. And across the country councils have been quick to mobilise in order to address the specific economic issues that they face in their areas be this related to major industries such as airport focussed economies, high street challenges or the visitor and culture economy.
There are significant challenges ahead. Although the Government has provided an unprecedented package of fiscal support to the country this cannot end with the conclusion of the roadmap. There will be a continued need for an ambitious programme of financial stimulus over several years. The Government has acknowledged this through recent funding announcements such as the £4.8 billion Levelling Up Fund and the £220 million Community Renewal Fund. Councils must play a central role in how these funds are best spent locally.
As the furlough scheme ends, no community will be untouched by unemployment. It is vitally important that a joined-up, place-based employment, skills and careers system offers adults and young people the recovery they deserve by providing access to quality education and training opportunities. Even before the impact of the pandemic, the nature of work was changing. The Government’s 2050 carbon net zero target will be a key driver of change in the UK economy. There will also continue to be greater demand for people to work in the healthcare and building sectors. New housing will play a vital role in the economic recovery of our cities, towns and villages and the need to decarbonise our housing stock will require a newly trained workforce. Consequently, it is going to be essential for both local and national Government to understand how employer demand is changing and how we can support local areas to adapt their skills profile to match the jobs of the future (see our green jobs report).
COVID has shown us the interdependence between successful economies and the infrastructure needed to support them. During the pandemic access to effective broadband services has become essential to facilitating working from home. However, 17 per cent of rural residential premises and 30 per cent of rural commercial premises still do not have access to superfast broadband (30 Mbit/s or higher).
The fragility of the public transport system has also come to light as an absence of users brings huge financial challenges to the future viability of services which are a lifeline for many. The future of office spaces is still unclear and could ultimately reshape the face of town centres over the next few years if commercial space gets converted into residential properties. These sorts of changes will directly impact on a whole range of businesses, including microbusinesses like Florence’s and their scope to exist in the future. This wide range of infrastructure challenges is going to need to be dealt with by a number of partners, as we recover.
The effects of the pandemic have mirrored, and in some cases exacerbated, our entrenched health and social inequalities. Never has the interdependence between health and the economy been closer, or the need for a fairer and more inclusive economic system been clearer. Many of the so-called health determinants are in fact economic determinants: the goals of developing the local economy, including the provision of good quality housing, to be more sustainable and productive, and of improving the health of the local population and reducing health inequality, are interdependent. Health, wellbeing and economic objectives should be explicitly aligned as part of a strategic approach to the local economy.
The pandemic abruptly stopped millions of people travelling and has changed the time and manner of journeys people make. New pressures on the transport system are congested roads at off-peak times and under capacity public transport. The pandemic proved that local government control and influence of buses provides for better and more efficient services that helped keep key workers moving even during the worst of the lockdown. The pandemic coincided with a watershed moment for local transport. Genuinely ambitious local bus service improvement plans and local cycling and walking infrastructure plans will soon be due, transforming the regulation of public transport and reallocation of road space across towns and cities. At the same time councils will get new powers long held in London, moving traffic offences and pavement parking restrictions. National and local ambitions to level up public transport quality and hit net zero will require significant, permanent and flexible resources to coordinate plans and deliver improvements to minimise the unavoidable permanent and intended changes to travel patterns and modes.
There are still too many out-of-date pieces of legislation that hamper councils’ ability to support Government priorities. For example, the outdated requirement to publish public notices in local newspapers. By allowing councils more local flexibility, they are better able to target vital information to their communities. This was clearly demonstrated during the pandemic. Councils were able to communicate and target information about vaccines and wider messaging about the pandemic, which helped to support the Government’s public information campaign and the deliver the successful vaccination programme. If the same restrictions had been in place as they are for public notices, this would have severely hampered councils’ ability to communicate and, importantly, to target messages in the most appropriate way.
During the pandemic, virtual meetings brought a number of benefits including many examples of increased participation rates in the democratic planning process, as well as reducing the need to travel to meetings and cost savings. Councils want to capture the benefits from this accelerated use of technology during the pandemic and should be given the flexibility to hold meetings virtually to bring a variety of benefits. The Government decision to end virtual meetings from 7 May should be reversed.
So how can we deliver a recovery which works for everyone?
Councils can work with Government to deliver an ambitious programme of financial stimulus, and have the knowledge and expertise to direct funds where they will have the most immediate impact to protect jobs and livelihoods and support long-term transformation of the economy, infrastructure and services.
Local economies are different and will need different things to stimulate them. Some require greater connectivity, some need to transition to new industries and others are short of affordable housing. Understanding the exact nature of an effective and sustainable stimulus can only be carried out locally. Councils are ambitious and optimistic about local prospects, while anticipating and mitigating risks and tackling inequalities where possible. (See our local economic recovery planning work.)
In turn these decisions can only be taken by empowered local decision makers who know what resources they can expect for the long term, including from the UK Shared Prosperity Fund, and the flexibility to use them in a way that makes sense locally. The scale of the challenge ahead means that a new approach to growth and policy responsibility is now required, one that matches the place leadership of councils and their crucial role in convening wider investment in public service with the need for locally tailored reconstruction and renewal.
It is welcome that councils have been given a leading role in the delivery of the Levelling Up Fund, but there must be greater devolution to councils for it to be truly successful. Local leaders need the powers and resources to bring government departments and agencies together to deliver locally determined and democratically accountable outcomes. Devolving economic powers means that local and regional leaders can use their local knowledge and their integration into the local community to utilise resources more efficiently and develop partnerships to grow their economies. Local leaders are better able to innovate to make the places they represent more inclusive through progressive procurement, living wage areas or anchor institutions.
Local government can also provide an essential focus on the microbusiness sector. Representing more than 2.1 million businesses just like Florence’s, and 33 per cent of employment in England, their growth has outpaced that of larger companies over the last decade. These businesses are the lifeblood of our communities. High numbers of micro retailers in urban environments and market towns, tourism businesses in rural areas and places of natural beauty, and an increase in overall numbers of public administration and health and social care businesses all contribute.
Worryingly, recent evidence from the Office of National Statistics shows that during the pandemic microbusinesses were more impacted than businesses of any other size. With nearly 10 per cent more facing temporary or permanent closure and micros representing 89.7 per cent of the total enterprises in England, it could have a detrimental effect on employment and the resilience of our communities.
On the surface, the pre-and post-pandemic challenges faced by microbusinesses up and down the country are similar, such as access to funding and support, employment and HR, marketing and communications, and other wider, mainly external factors. There is also an added level of complexity; business owners with no or few digital skills have struggled the most as the world has become increasingly online and cashflow even more limited as lending reduces.
We can provide evidence and strategic thinking alongside our partners in business support organisations and a leadership role in ensuring the support on offer is relevant locally. We can use our significant spending power to ensure social value can be directed towards micro, small and medium-sized businesses. Finally, we can use our regulatory role to support planning to provide affordable and suitable workspace and licensing powers to encourage growth of our local markets and sectors such as hospitality and creative and cultural businesses.
There is a real opportunity here for councils to address broader issues around inequality through economic recovery. Microbusinesses are extremely diverse across age, gender, ethnicity, sector and industry. The understanding that councils have of their microbusiness community enables them to provide direct support to disadvantaged groups. For example. the Marches Growth Hub (covering Herefordshire, Shropshire, Telford and Wrekin) highlighted that during the pandemic they received an increase in queries from taxi-drivers of Asian ethnicity asking for assistance with grants due to English not being their first language. Salford City Council has launched ‘The Salford Way’ project which is focussed on tackling inequality through economic development. These projects illustrate the targeted benefit councils can deliver around inequality through their economic recovery work.
If we build back local, we can create economies fit for the future and support businesses, just like Florence’s and to ensure everyone in our communities is skilled up for the jobs of the future.
This can be delivered through an evolved relationship between local and national government. One which respects the direction set nationally for the economy by the Government. But also recognises that this direction is best achieved by devolving delivery to local decision makers. If we get it right, we can reposition our economies to be on the front foot and remain ready for whatever challenges the future may hold.
Economic recovery: sector support at a glance
We have provided councils with a raft of support to mitigate the varied economic effects of the crisis.
We supported councils in the distribution of the Small Business Grants Fund and Retail, Hospitality and Leisure Business Grants Fund schemes, which helped to stimulate local economies and support businesses to survive. We have also worked with Local Partnerships to support councils and the sustainability of their leisure providers and produced a town centres toolkit, which includes guidance to support councils and place partnerships to develop COVID-19 recovery planning as part of wider revitalisation.
One Public Estate
The One Public Estate (OPE) programme is an established national programme delivered in partnership by the LGA and the Office of Government Property within the Cabinet Office. OPE’s networks and intelligence provided critical COVID-19 response support in the early stages of the pandemic. OPE provided support to MHCLG’s Housing Delivery team through the continued delivery of the LRF1 programme, wider public land project delivery intelligence from the OPE programme, and through support for the design of emerging place-based housing delivery funds – including the Brownfield Land Release Fund, which launched during early 2021/22. The OPE programme also delivered the MHCLG-sponsored OPE Phase 8 and LRF2. This involved the launch of revenue and capital funding offers, for all English local authorities. OPE8 provided £10 million of revenue support to rationalise, co-locate and repurpose surplus public land, while LRF2 provided £20 million of capital funding to bring surplus local authority land forwards for housing delivery. Further, OPE provided wider support to MHCLG by inputting into the moderation of bids submitted to the Future High Streets Fund, purposed to renew and reshape town centres and high streets in ways that drive growth, improve experience and ensure future sustainability.
Net zero
This pen portrait is an imagined experience, based on the interaction between residents and councils and councillors across the country.
Raj is 15 years old and lives at home with his parents and younger sibling
I’ve been interested in climate change for a while now. I can’t believe how many more stories there are about bad floods or forest fires across the world. I get a lot of information about it online. Me and my mates went on a climate strike. There was a really good atmosphere. Lots of us all saying the same thing. We need change now, not tomorrow. Everyone was starting to pay attention to what young people were saying and Greta Thunberg was all over the news.But then COVID happened. We all ended up stuck at home. And now everything is about the virus. It’s like we lost all that focus. Decision makers can focus when they need to, COVID has shown us that. Everyone has got together to make massive changes in lockdown and to stop COVID spreading. We now need decision makers to focus on climate change as well. In the same way that they made big decisions overnight to fight the pandemic they now need to make big decisions to protect us from climate change.
I know COVID is still a concern. But the climate is also really important. It’s been young people who have made the world realise that we can’t just ignore what’s being done to the planet. It’s weird because adults are meant to be our role models but it’s us young ones who are leading the way on this. We are making people look at climate issues differently. We are driving the change. Adults need to step up now and deliver. There is no planet B.
Delivering during COVID
Prior to COVID-19, net zero was high on the public and political agenda. Local government has a long history of being involved in net zero issues: More than 300 councils signed up to the Nottingham declaration on climate change back in 2000 and more recently over 230 councils have declared a climate emergency. Many councils have worked on specific projects to address net zero issues and some such as Bristol, Manchester, Nottingham and Leeds have developed significant climate change programmes.
Throughout the pandemic, councils have continued their commitment to dealing with net zero. Lockdown resulted in an increase in household waste as we all consumed more from home. Waste and recycling collections continued with minimal disruption throughout the various lockdowns. Councils have ramped up their investment in cycling and walking infrastructure giving residents greener options and 99 per cent of councils kept their parks open so that residents had access to clean green spaces.
Councils have also supported the role of electric vehicles by investing in on and off-street electric vehicle (EV) charging infrastructure – contributing to the 21,000 public charge-points across the UK. Birmingham City Council has brought the first Clean Air Zone into operation which by 2026, is estimated to reduce the number of asthmatic children showing bronchitis symptoms by 873 a year. It will also contribute towards Birmingham’s committed 60 per cent reduction in carbon emissions by 2027. Given that it is the single largest source of emissions in this country, transport has a significant role to play in helping the country to reach its net zero targets.
Two thirds of councils want to be carbon neutral by 2030. But Raj is right, issues like net zero which need difficult decisions can run the risk of becoming secondary issues to the pandemic. With the right local leadership communities can use the recovery to progress to a more sustainable future which brings with it greater opportunities for jobs and an improved quality of life.
The Government has legislated to reduce carbon emissions by 78 per cent by 2035, and to reach net zero by 2050. This is an ambitious target which will require significant change across society. It is important to address the challenges which lie ahead and often get in the way of delivering the sort of change people like Raj expect in the future.
To achieve these goals, Government will need to build effective partnerships to broker deals across a range of sectors. Locally, councils can do a similar thing. They have existing relationships with a whole host of partners which they can use to help deliver the individual changes needed to meet the national target. Already areas such as Yorkshire and Humber and Hertfordshire have climate change partnerships involving their local NHS and other major partners to look at how they can collectively deliver emissions targets.
The Government rightly recognises that the transition to a net zero future requires an enormous shift in the global financial system by identifying finance as one of the four COP 26 goals. This is a positive step to mobilise investment from both the public and private sectors. However, it will be important that financial investment led at the international and national scale is translated into the delivery of locally-led solutions. Councils know their places and communities but need long-term certainty and local flexibility of funding to create a net zero future. This will enable them to plan much more effectively and holistically. Local government is ready to work with national government to maximise the outcome from any additional funding and to work with partners to ensure that everyone is contributing towards the investment that is needed. Ensuring producers pay for the waste they create is a step in the right direction, ensuring that the cost of processing waste is borne by those who have created it.
To deliver significant progress on net zero it is going to be necessary to ask the public to make further behavioural changes. We have already made some of the easier changes, such as swapping to reusable shopping bags/water bottles and getting better at recycling. But the next phase of behavioural change is going to need more commitment from the public as we look to swap our modes of transport and seriously review our own personal consumption. The Committee on Climate Change estimates that future reductions in emissions will rely on as much as 62 per cent of our individual choices and behaviours.
However, councils have a strong track record of being able to lead on exactly this sort of behavioural change. Waltham Forest Council is just one of the many councils which has been proactive in developing their response to air quality issues. Sometimes this involved local politicians working with local communities to make unpopular short-term choices in order to deliver longer-term benefits. The council has delivered 27km of cycle track, 15 new pocket parks, over 100 new safer junctions. As a result cycling has increased 103 per cent and car usage has dropped 7 per cent.
So how can we work with local communities to reach the net zero target?
Although there are significant challenges ahead there are also many opportunities available if national and local government work together. Councils want to work as essential partners with Government to tackle climate change.
Councils are fundamental to transitioning our places and empowering our communities and businesses to a net zero future. They are well-placed to translate national climate ambitions into transformative action on the ground through:
- Councils' place shaping role
Places are intrinsically local and councils are the master planners. Local planning authorities not only deliver quality homes, but shape environments that are sustainable and ensure people have access to the right infrastructure, transport, connectivity and services. Some councils are already doing this by developing ’15-minute cities’ to improve quality of life, strengthen high streets and create options for more sustainable lifestyles. Although councils’ own direct emissions account for approximately 2 per cent of total emissions, they can influence up to 70 per cent of emissions in their local places.
- Purchasing powers and market shaping
Procurement is a key power that councils have to deliver net zero. Through commissioning, councils bring together public, private and voluntary partners to shape the market to best meet the needs of communities. In 2019/20 their third party spend was at least £63 billion, mobilising private investment into net zero delivery and building capacity in the market for low carbon goods and services.
- Problem solving and direct delivery
Different localities have different geographies, demographics, infrastructure and resources. Councils have demonstrated an ability to capitalise on local assets and opportunities to find local solutions to local challenges. They provide a repository of local knowledge and understanding essential to the delivery of net zero solutions on the ground, pilot innovative projects to help reduce the risks, develop new business models, test alternative technologies, and drive the wider roll out and scaling up of low carbon solutions.
- Utilising council assets
Councils are landlords and significant asset-owners. Many councils have their own building stock, whether that’s council-owned housing or commercial and institutional buildings such as retail units, schools and leisure centres. They are also considerable landowners in the UK. They provide existing pipelines of infrastructure for shovel ready carbon reduction projects in buildings and are early adopters to test new technologies.
- Role as convenors and communicators
Councils are convenors and communicators for businesses and civil society. Their responsibilities as frontline service providers and strategic place makers mean that councils have a longstanding ability to collaborate and build cohesion with local partners and residents, including the most vulnerable. Community capacity and cohesion issues will arise in the transition to net zero and it is only at the local level that these can be addressed.
Local government can support the Government’s ambition by empowering communities and vulnerable groups to mitigate and adapt to climate change. Their strength comes in being able to translate national climate messages locally, reaching the more difficult to engage, and building public consent for the likely disruptive changes which will come with the transition to net zero.
If we build back local now, we can meet the targets and ambitions of Raj’s generation to deliver net zero.
A clear national climate change framework which enables local councils and their partners to deliver on the ground can help the country move forward into a greener future. One which is more sustainable. There is a real opportunity now to use our recovery from the pandemic to reset our approach to net zero. Local councils are ready to play their part in this journey.
Net zero: sector support at a glance
Our Climate Change programme has been extremely well used, with 90 per cent of councils in England and Wales having engaged with the support offer. The programme offers a Greenhouse Gas Accounting Tool, designed with Local Partnerships, which provides councils with a means to measure emissions and compare impacts in a standardised way. The tool has been downloaded by over 200 councils and was endorsed by the Climate Change Committee, which advises the UK Government on tackling and preparing for climate change.
The Net Zero Innovation programme, delivered in collaboration with University College London (UCL), supports councils to address local climate challenges by bringing together local authorities, universities and other stakeholders.
Housing, planning and building safety
This pen portrait is an imagined experience, based on the interaction between residents and councils and councillors across the country.
Steve, 45, lives with his wife and two teenage children
We have been in this flat on this estate for years. I know everyone. We are like a big family. We all look out for each other and if you need help someone will give it. But things are changing.My kids are getting older now and they need more space. My parents are also aging and at some point will need help. They have offered to sell their property so that we could all live together. I need a house that will give us more space but can also accommodate older people.
And I want it to be somewhere we can all live in for a long time. Not one of these flimsy houses that modern developers just build overnight. I need a real family house. Something built to last. Good quality and safe. But something we can also afford. I don’t want to have to move miles away from everything I know. Sometimes it feels like lots of new housing is being built, but it’s not really for people like me. Families like us need our housing to be close to schools, doctors and parks. If we are going to level up then my family deserves the same quality of life as other families.
Delivering during COVID
Local government shares the Government’s ambition of delivering 300,000 new homes a year, but the dreams of families like Steve’s can only be delivered through national/local partnerships. As house builders and landlords; as planners, place-shapers, and agents of housing delivery, growth, transport and infrastructure; as responsible guardians to the vulnerable and the homeless; and as democratically accountable to communities – local government is at the heart of the housing solution.
During the COVID-19 crisis, councils responded rapidly to support the homeless through the Everyone In initiative. Based on MHCLG figures, by the end of 2020, councils almost immediately moved an estimated 90 per cent of rough sleepers into hotels, bed and breakfasts and other temporary accommodation. Altogether councils supported over 37,000 individuals, with more than 26,000 now moved on to longer-term accommodation. This demonstrated that given the mandate and funding, councils, working with their partners, have the means to end the vast majority of rough sleeping. Virtual planning committees were one of the most significant changes for planning departments. By June 2020 around 70 per cent of authorities had undertaken one or more virtual planning committees, with more planned. Councils must be given the flexibility to continue to hold these meetings, to harness digital technology and support wider engagement in the planning process, as well as mitigating climate change.
In March 2021 we helped to secure a series of Right to Buy reforms giving councils increased flexibilities to build more homes. This included: extending the time councils have to spend Right to Buy receipts from three to five years; an increased cap in the percentage cost of new homes councils can fund from Right to Buy receipts, raised from 30 per cent to 40 per cent; and allowing receipts to be used for shared ownership, First Homes, as well as affordable and social housing. Alongside this, the government also introduced a cap on the use of Right to Buy receipts for acquisitions.
As communities move towards recovery there is a real opportunity to deliver a better future with greater levelling up. If correctly addressed the housing and planning agendas can collectively shape better places to live which can offer better jobs, sustainable living and access to communities where local people are leading good quality lives. The vision Steve has for his family isn’t unrealistic, but challenges need to be addressed.
The pandemic has highlighted health inequalities due to insufficient access to green space and poorly designed homes and places. A key part of delivering a recovery for all is more quality homes in the right places and the supporting infrastructure to create sustainable, resilient places. It is vital that we build more homes for social rent. This will help us tackle our housing crisis and reduce rising levels of homelessness, improving people's health and wellbeing while alleviating the pressure on health and social care.
The planning system is not perfect. It needs to be simplified and updated with the better use of technology. Ensuring that developers build high quality homes in a timely way once planning permissions are given is also essential. The new planning system proposals, set out in the ‘Planning for the Future’ white paper, provide for a much greater use of digital technology which should provide better access and transparency for communities. We await the publication of the Planning Bill, but any reforms will have to provide for a locally-led and properly resourced planning system in which councils and the communities they represent have a say over the way places develop. In this way we will ensure the delivery of high quality affordable homes with the necessary infrastructure to create sustainable, resilient places for current and future generations. It is also crucial that housing is not planned in isolation, but considered alongside economic growth and jobs.
There must be full community involvement in planning, and a strong focus not just on housing numbers and speed of delivery, but on developing sustainable communities that includes a much wider remit. For people like Steve this includes job creation, economic development, tackling climate change, improving biodiversity and infrastructure delivery. Councils need to have the tools, powers and flexibilities required to plan for and deliver the quality homes and places communities need.
Communities across the country have already potentially lost 16,200 affordable homes through office to residential conversions. New permitted development rights (PDR) introduced during COVID will further undermine much needed affordable housing. COVID has highlighted stark inequalities within our society, especially so in health outcomes due in part to poor quality housing such as that developed through existing PDR, leading to poor ventilation, a lack of space standards, and a lack of access to services and green space.
How can we deliver homes fit for the future?
There is a unique opportunity to address these challenges as we come out of the pandemic and offer a broader vision to our communities. If both local and national government work with partners there is a greater chance of delivering at the pace local communities need but with a much broader vision around place. We can deliver the kinds of places people like Steve want – tailored to the needs of their local areas. This can help to level up across a number of socio/economic factors:
- Planning
The number of homes granted planning permission has far outpaced the number of homes being built. Latest figures show that 2,782,300 homes have been granted planning permission by councils since 2010/11 but over the same period only 1,627,730 have been built. There is also land for more than one million homes already allocated in Local Plans which developers have not yet brought forward to planning application stage. Councils need powers to tackle our housing backlog and step in where a site with planning permission lies dormant and house building has stalled. This includes the ability to charge developers a full council tax for every unbuilt home where it is not built to agreed timescales. Councils should also have streamlined compulsory purchase powers to acquire stalled housing sites or sites where developers do not build out fast enough.
Planning fees do not cover the true cost of processing planning applications, and taxpayers currently subsidise the cost at a rate of nearly £180 million a year. Between 2010/11 and 2017/18 there was a 37.9 per cent fall in net current expenditure on planning functions and planning departments. This significantly reduces their capacity to ensure the delivery of new housing through the planning process and enable the new supply of housing and appropriate infrastructure. Council planning departments could become self-financing by allowing councils to set planning fees locally.
The Government’s proposals to shift to a more digitalised planning system (local plans online) makes the planning system more accessible and efficient. Councils will need the appropriate resourcing to lead on this step-change and issues of digital exclusion will need to be addressed to ensure all residents can engage in the planning process. Virtual planning committees should recommence, making planning meetings accessible to all especially to those who are less able to get to physical meetings.
The new Local Plan process and timeframes need to allow the time and resources required to undertake a mix of genuine forms of engagement where the digital approach is either not the best, or not a possible option. Councils should have the flexibility to determine the most appropriate way of engaging with the public that provide easier and more cost-effective ways of finding out about, for example, planning applications and planning decisions.
A real partnership between central and local government around planning could deliver significant change which helps the system to deliver more house building. - Housing
Councils can play an important role in rebuilding the national economy following the pandemic, by building new homes for social rent. A programme of building 100,000 new homes for social rent each year will help economic recovery and deliver long-term fiscal benefits. This would meet demand for affordable homes and deliver a £14.5 billion boost to the economy, including jobs, and would yield a net present value public sector surplus of £7.8 billion over 25 years and a real annual return to government of 3.8 per cent each year.
Our council housing stimulus package outlines the key policy and fiscal interventions that would have a positive impact in stimulating an increase in the supply of council housing and includes a long-term rent deal for landlords, 100 per cent retention of Right to Buy receipts and additional capacity. Expansion of the development programmes of councils would offer a pathway out of expensive and insecure private renting, and on towards ownership and over time, reduce the cost to Government of meeting the housing needs of low-income households through reductions in the housing benefit bill. In addition it would make a major contribution to the Government’s ambition of 300,000 new homes a year, help address pressure on public services, notably health and social care, driven by poor housing conditions, support the re-purposing of town and city centres as well as enabling people to remain in rural areas in which they grew up and support a climate smart recovery. - Achieving net zero
Local government has been leading the way on innovative and collaborative approaches to achieving net zero housing. This includes through the housing advisers sector support offer and leading the way on our net zero ambitions by decarbonising housing and delivering carbon neutral housing. Examples include improving housing standards through exemplar innovative approaches to housebuilding such as the Passivhaus Social scheme.
- Safety
Four years on from the Grenfell Tower fire, thousands of residents are still living in buildings with serious fire safety defects and the new building safety regime has yet to emerge. Councils and housing associations were generally quick to address cladding concerns but progress in the private sector has been unacceptably slow and despite the provision of £5 billion in Government support, hundreds of thousands of leaseholders still face the prospect of unaffordable bills for industry’s failures.
We lobbied for a lowering of the height at which sprinklers are required in new buildings and a ban on combustible cladding on buildings over 18 metres. The Government has committed to lower the height at which the cladding ban takes effect, should provide support to retrofit sprinklers in socially-owned blocks, and to protect leaseholders from the cost of rectifying fire safety issues that are not their fault. Four years on, there can be no further delays in introducing the new safety regime. That regime, which will depend on councils and fire services to deliver its functions, will need adequate funding if it is to be effective. There is a significant lack of building control, environmental health and fire engineering capacity in the UK which needs to be addressed if the regime is to work. As the new regulator is still some two years away from commencing operations councils and fire services need to be supported in their enforcement roles in the meantime.
If we build back local, we can truly level up and provide the sorts of houses that families like Steve’s want to live in.
The longer-term ambition has to be to deliver local areas that have high quality affordable homes built in the right places, supported by the right infrastructure, which provide enough schools, promote greener and more active travel, and tackle climate change. This will need a national/local partnership which starts with a locally-led planning approach with public participation at its heart.
Housing, planning and building safety: sector support at a glance
When the pandemic hit, councils and their partners worked tirelessly to support rough sleepers under the aegis of the Everyone In initiative. Working together with MHCLG, we developed and facilitated a Rough Sleeping Peer Support offer to assist councils in their rough sleeping response. Our programme of delivery and impact panels provided council lead officers with a safe space to come together, share and challenge knowledge and learning, and highlight good practice from across the sector.
Since the first panel in December 2020, 239 councils have benefited from this programme, with an average of 88 per cent of participants saying they would be likely, or very likely, to recommend a rough sleeping panel to another council. We will shortly be publishing a report which captures the key themes and emerging learning from the panel discussions – capturing the voice of the sector and those directly involved in the effort to safely accommodate rough sleepers at a time of national crisis.
Council finance
This pen portrait is an imagined experience, based on the interaction between residents and councils and councillors across the country.
Sam is 27, they live alone
To be honest I don’t really think about the council in my day-to-day life much – other than when my council tax bill comes. I’m pretty self-sufficient, so I can look after myself. When lockdown happened, I knew I’d be okay. But it was the little things that I started to notice. The bins kept on getting collected – without fail. I had a lot more rubbish because I was at home all the time. My neighbour seemed to be going to the local tip a lot so that must have stayed open too.My local park made a huge difference for both my mental and physical health – it was where I could get fresh air, exercise, and go on walks with friends. If it hadn’t been open, the lockdowns would have been unbearable. I worked from home throughout the pandemic; I am lucky to have a secure job in accountancy which allowed me to do that. I live on my own in a flat without access to an outdoor space or balcony, so at times during lockdown I felt really lonely and a bit claustrophobic.
I guess your council isn’t really something you think about a lot unless you need something. But it was good to know that they were able to do all that sort of stuff. I don’t really want to have to think about all the council’s different services and how they get funded. I just want to know that when I need help I will get it. Especially when you get older and can’t do everything for yourself. I want to know that there will still be people there to help me when I eventually need it.
Delivering during COVID
During the pandemic, councils across the country acted swiftly, completely reshaping their services to support their communities’ immediate needs and reconfiguring their systems to deliver the Government’s national strategy with short notice. Since March 2020, councils have distributed tens of billions in support for businesses and supported residents with hardship funding where they struggled to meet their council tax bills.
Despite the scale of the challenge, local government dealt with the financial impact well. Surveys suggest that councils managed over £8 billion of additional cost pressures and £3 billion of lost income, excluding business rates and council tax, since the pandemic began. It is welcome that the Government compensated a significant portion of this, but this needs to continue to be monitored and funded if additional pressures arise.While some councils have experienced financial difficulties, which required further exceptional support, overall the skilled management of finances ensured that local government could continue to deliver services for residents even through the most difficult times.
Looking ahead, there are several challenges facing council finances:
Uncertainty
For the fourth year in a row, councils are facing significant uncertainty over funding for next year, both nationally due to one-year spending reviews and local government settlements, and locally due to the uncertainty around the future of further business rates retention and fair funding review reforms. This is furthered hindered by the significant uncertainty surrounding business rates as a council source of income due to an ongoing fundamental review as a result the pandemic. This ‘financial cliff edge’, hinders councils’ ability to plan ahead, something which is crucial to deliver investment, valued local services and support vulnerable residents. Under the current situation, councils are likely to plan for a worse future, which can lead to service reductions and redundancies which are actually not required, than they would if they had certainty.
Spending power
Council budgets are under continued financial strain. After a decade which saw a reduction of £15 billion in core government grant funding, the Government’s preferred route to increase council funds is through council tax. Around 85 per cent of the Government’s projected increase in council core spending power in 2021/22 was based on the assumption of all councils increasing council tax to the maximum allowable amount (for example, 5 per cent for social care authorities). While council tax is an important funding stream, it raises different amounts in different areas not related to need and puts more pressure on local taxpayers for what is a national issue. Additional funds delivered through other routes, such as grants, are minor by comparison (other than COVID-19 funds).
With the future need to stabilise public finances, councils will continue to face challenges and will have to prioritise less visible but highly valued local services, such as social care. Our early analysis ahead of the forthcoming Spending Review shows that councils face average annual cost pressures of £2.5 billion to maintain services at their current level of access and quality. Of this, £1.1 billion per year is related to adult social care in addition to a £1.4 billion provider market pressure. This shows that unless adult social care funding is fundamentally fixed, councils will always be under financial pressure.
Fragmentation
Council funding is also increasingly fragmented. Even prior to the pandemic – which itself came with a myriad of different funding pots and schemes – LGA research shows that in 2017/18, nearly 250 different grants were provided to local government. Half of these grants were worth £10 million or less nationally. At the same time, these grants are highly specific – 82 per cent of the grants are intended for a specific service area. Around a third are awarded on a competitive basis and the small value of grants means that more can be spent by councils on preparing bids than is received back.
So, how can we move towards a more sustainable local government finance system?
The upcoming Spending Review is a chance for the Government to provide local government with the right framework to be able to support it in its levelling up ambitions.
- By delivering a multi-year Spending Review followed by a multi-year local government finance settlement, combined with clarity over the future of local government finance reforms such as the fair funding review, giving councils the certainty they desperately need.
- Through further grant funding or the devolution of tax, the 2021 Spending Review should deliver a sustainable financial settlement which does not see residents paying more council tax without an increase in services provided.
- By joining up and streamlining fragmented funding into larger, flexible-use pots, the system of local government funding can provide much better value for the same amount of funding.
If we build back local, we can resource effective local services for people like Sam and their community.
Councils’ pandemic response has shown the need for and impressive impact of well-resourced, efficient and effective local services. To best deliver for their residents, and by doing so maximise their contribution to the nation’s economic and social recovery, council services need certainty together with sufficient and sustainable funding.
Council finance: sector support at a glance
We have provided councils across the country with much-needed support to help mitigate the financial effects of the pandemic – principally through the Finance Improvement and Sustainability (FISA) programme, which uses experienced advisers whose role it is to provide advice and insight to councils facing financial challenges. With the number of councils experiencing financial issues growing substantially during this period, FISAs have provided direct support to 67 councils since the beginning of the pandemic. Support from FISAs has helped councils to understand and monitor the impact of COVID-19 on their finances; identify options for seeking in-year savings and alternative funding strategies; deliver financial planning for recovery and renewal; and support individual chief finance officers in undertaking their duties.
The programme has also provided councils access to collaborative finance panels (CFP). The CFP is a part of our wider financial resilience offer and not only serves as a platform for sharing information but also a learning network where issues and concerns are discussed in a supportive and constructive environment. In the past year, it has brought together groups of councils to reflect and learn from their responses to COVID-19.
The next step – valuing local difference
Whether we are working at a national or local level, people and the places they live in remain at the heart of what we do. We share an ambition to deliver services which empower people and give them choice. But the pandemic has thrown up real challenges to this. COVID has laid bare the complexity of people’s lives and the interrelated nature of problems.
As we move towards a new future there is a shared sense between national and local government that no one should be falling behind. We should be levelling up for everyone, no matter where they live, and that will require a focus across a range of economic, social and health related factors. The joint endeavour which is needed to do this will be unique. Our country faces a moment the likes of which none of us have lived through before, and places will need to draw together bespoke packages of support to help them recover.
Councils have been a trusted partner to Government to deliver throughout the pandemic. As elected representatives, they have the democratic mandate to work with Government and local partners to support all local communities. They remain committed to delivering for everyone into recovery. Local government recognises that Government will set the national direction of recovery through key fiscal tools and national policy. As part of this partnership, the trust should be extended to allow councils to deliver recovery locally and to join up initiatives and funding in a way that has the greatest impact for local communities.
What this looks like will vary from place to place. What we need to do is value this local difference. Value local, political, leadership.
Valuing and understanding local difference is what will truly enable us to level up. It will deliver the targeted change on the ground which will directly improve people’s lives. Whether this be specialised health services, new green jobs or better-quality housing. As our portraits have shown councils can offer a complex range of support to help deliver all these ambitions for local people.
We can collectively deliver better outcomes where there is a genuine partnership. A partnership between local and national government based upon early involvement in policy development, effective sharing of meaningful data and open conversations about future funding challenges and how we can work to resolve them.
As we move forward, enabling local people to make local decisions will create the conditions for sustainable growth, better public services and a stronger society. Now is the time to fully commit to a national and local partnership which can deliver for future needs. Now is the time to recognise and value local difference as the solution not the problem.
Now is the moment to build back local to ensure people and places remain at the heart of the recovery so that we level up and no one is left behind.