Background and introduction
The Insight Project was developed to create a national picture regarding safeguarding adults’ activity during the COVID-19 pandemic. The first report, COVID-19 Adult Safeguarding Insight Project: Findings and Discussion, provided a picture of how safeguarding adults activity in England was affected by the initial stage of the pandemic and first lockdown, up until June 2020. The COVID-19 adult safeguarding insight project second report provides information on safeguarding adults activity up to December 2020. This third report covers the period up to June 2021.
Key messages from the third Insight Report
- The third Insight Report summarises safeguarding adult’s activity data and information from 106 Councils in England.
- Fifty councils shared qualitative insight in the third project.
- Safeguarding concerns continue to show a long-term upward trend, tending to decrease during periods of lockdown and other COVID-19 restrictions followed by a sharp increase once those restrictions are lifted.
- Section 42 safeguarding enquiries did not show the same upward trend shown by concerns, though they did fall and rise in line with changes in the volume of concerns.
- Variation between local authorities in the volume of safeguarding concerns and Section 42 enquiries has been and remains high, as local authorities respond to differing circumstances in their local areas.
- Due to lockdown regulations, many safeguarding concerns have been reported to adult social care services later than prior to the pandemic. This has been the case for particular types of abuse, such domestic abuse and self-neglect where lockdowns have increased the isolation of those experiencing abuse.
- The delays in reporting safeguarding concerns or related issues have altered how they have been dealt with since the pandemic. Delayed issues are less likely to be case managed, instead becoming safeguarding concerns. Delays in referral have meant that there have been more acute or severe consequences, making preventative measures more difficult to implement or situations have been more likely to require crisis management.
- Prevalence of different types of abuse has not changed considerably during the pandemic, although there is some limited evidence in the data that psychological abuse, domestic abuse and self-neglect have risen during this time. However, councils have reported increased complexity and risks in abuse types.
- The pandemic has created additional layers of complexity for safeguarding practice, ranging from how practitioners work during lockdown to the ‘Everyone In’ initiative regarding people experiencing homelessness. Additional issues such as substance misuse, mental health problems, reduced/no access to care and support services during the lockdowns have provided additional challenges.
- The location of risk in the individual’s own home has increased notably during the pandemic, with risks located in residential and nursing care homes conversely making up a lower percentage share of Section 42 enquiries.
- Prevalence of different outcomes of enquiries has remained more or less constant throughout the period recorded, although during lockdown periods there have been slight increases in the percentage of enquiries with the outcome of “Risk Reduced”, as opposed to “Risk Removed” or “Risk Remained”.
- During the pandemic period there has been a distinct decline in the rate of individuals aged 85 and over involved in Section 42 enquiries, with other older age groups experiencing lesser declines and the rate of individuals aged 18 to 64 experiencing a slight increase.
- The mental capacity of adults at risk has remained virtually unchanged in the pandemic period compared with previous years.
- The risk identification and action taken of Section 42 enquiries has remained almost constant in the pandemic period compared with previous years; though with a subtle decrease in the percentage of enquiries with risk identified and action taken.
- Councils reported on the impact of COVID-19 on work with social care providers; increasing mental health issues; abuse of people with learning disabilities, safeguarding people experiencing homelessness, and carers’ stress.
- Technology has had a significant impact on ways of working, opening up increased opportunities for multi-agency engagement with professionals and has had an impact on the safeguarding work with adults with care and support needs.
- Stronger and new partnerships and multi-agency working have been prominent features during the pandemic.
- Innovative and responsive services have developed in response to the challenges presented by the pandemic and lockdowns.
Rationale
The COVID-19 pandemic and accompanying lockdowns have had an unprecedented and extraordinary impact on all aspects of day-to-day life and behaviours. There are ongoing concerns about how people with care and support needs may experience different or more abuse or neglect due to these changes. Insight into the impact of the pandemic on safeguarding activity can firstly, describe what is happening, secondly, inform future activity to mitigate increased or different risks of abuse and thirdly, offer a national picture for the varied and shared local experiences. Data and intelligence provide evidence, both to emphasise the importance of safeguarding adults and influence policy and decision makers.
It is important to understand what has happened, and continues to happen, to respond to changing safeguarding needs, learn lessons for future COVID-19 outbreaks and consider the longer-term impact of the pandemic. It is hoped that this insight and data improve understanding of the impact of COVID-19 locally and nationally and informs responses to people with safeguarding needs as well as assist planning for the future. For example, this Insight Report can help councils respond to the action in the 2021/22 Winter plan for them to ‘review any systemic safeguarding concerns that have arisen during the pandemic period, and ensure actions are in place to respond to them, enabling readiness for any increased pressures over the winter period.
Throughout the pandemic, there have been concerns that safeguarding issues were not being identified and reported, due to reduced ‘face-to-face’ contact between adults with care and support needs and professionals, families and friends, especially, but not only, regarding people living in care homes. In community settings, there continued to be increased concern regarding the ongoing impact of social isolation and the changing risks of abuse for people with care and support needs (eg. increased self-neglect, new scams regarding COVID-19 testing and vaccination). There continue to be concerns about ‘surges’ in safeguarding demand and activity when lockdown restrictions are eased and face-to-face social and professional contact restarted and intensified. The monthly data, alongside the qualitative intelligence, collated in these Insight reports describes the median experience amongst councils but also how councils may have seen a very different set of patterns and trends.
The Safeguarding Annual Collection (SAC) is the annual mandatory data return for recording safeguarding activity operated by NHS Digital – captures information about safeguarding activity at the end of each financial year; the annual return for 2020/21 has been incorporated into the findings described in this report. This data does not provide a picture of changes during the year. The annual data shows how 2020/21 compares to 2019/20 but does not show how the different phases of the pandemic and lockdowns have impacted on safeguarding activity. This is the gap that the Insight reports aim to fill.
It was recognised that councils were, and continue to be, under considerable pressure to meet other mandatory data requests from central government during the COVID-19 pandemic, which meant it might be difficult to respond to the requests for safeguarding data. This Insight Project was therefore entirely voluntary and flexible. The proposal for the Insight Project has been supported by Local Government Association (LGA) and Association of Directors of Adult Social Services (ADASS), through the safeguarding workstream of the Adult Social Care Hub (joint LGA and ADASS), Care and Health Improvement Programme (CHIP) and with support from the co-Chairs of the National Principal Social Workers Network, safeguarding leads at the Department of Health and Social Care (DHSC) and the National Network of Chairs of Safeguarding Adults Boards.
Given the multiple variables that impact on safeguarding activity, inferring causal relationships and patterns that would apply to all councils is problematic. This report looks to indicators and factors that provide a narrative that show overall trends. It is intended to provide a national picture for strategic reflection, offer a framework for analysis of the local experience in comparison to the national trends described and capture the complexities of the impact of the pandemic on safeguarding activity in England during this period.
First Report findings: summary
The first report included information covering the period between January 2019 and June 2020, from 92 councils. This showed that safeguarding concerns dropped markedly during the initial weeks of the first COVID-19 lockdown period, only to return to and then exceed expected levels in June 2020. The trend of safeguarding enquiries showed a similar decline during the initial weeks of the COVID-19 lockdown period and upturn in June 2020, although the June upturn was not as great. This could have been due to several factors including: the time frames for undertaking and completing safeguarding (section 42) enquiries, lower levels of data contributions for June 2020; and activity in June not having caught up with the backlog of safeguarding concerns generated in the first lockdown period.
Section 42 enquiries’ refers to Section 42 (ii) of the safeguarding decision-making process described in the Care and Support Statutory Guidance, (2020) paragraphs 14.93-103. A Section 42 enquiry is an enquiry undertaken under Section 42 of the Care Act 2014, in response to indications of abuse or neglect in relation to an adult with care and support needs who is at risk of abuse or neglect and unable to protect themselves because of those needs.
Analysis of the percentage distribution of types of abuse within safeguarding enquiries indicated that domestic abuse increased slightly overall, and significantly within some councils, as well as slight increase in psychological abuse and self-neglect. The percentage of safeguarding enquiries where the risk is in the individual’s own home had increased markedly related to the confinement of people in their homes. Safeguarding enquiries where the risk/safeguarding incident was in care homes had decreased as a percentage over the same period, confirming fears that there was a reduction in activity and reporting due to lack of visiting and outside scrutiny in those environments during the first lockdown period.
Second report findings: summary
The Second Insight Report covered the period to December 2020 and summarised data and information from 101 councils in England. The key messages were that the COVID-19 pandemic and accompanying lockdowns had an unprecedented and extraordinary impact on safeguarding. Rates of safeguarding concerns during 2020 were overall higher than 2019. There continued to be a sharp decline in the rate of safeguarding concerns as lockdowns started, followed by steep increases immediately as lockdowns ended. These increases were often sustained until the following lockdown period. However, not all councils followed the national trends.
Councils who reported increased numbers of concerns during the lockdowns said that these were from emergency services, family, friends, neighbours, volunteers, and health partners. Only 29 per cent of councils who sent qualitative data saw no change. Nationally, there were moderate increases in the rates of domestic abuse, self-neglect and psychological abuse reported in safeguarding activity in 2020, compared to 2019.
Councils reported receiving a high level of safeguarding concerns regarding adults who did not have care and support needs, nevertheless they were at risk of multiple categories of abuse and neglect and they were supported without going down a safeguarding pathway.
Safeguarding enquiries increased in a person’s home during the lockdown period and overall, there was a decrease in safeguarding enquiries in both nursing and residential home settings during the pandemic period. Councils commented on reduced access by professionals, families, and friends to care homes. Increased levels of complexity in safeguarding activity undertaken were reported.
Councils described the challenges that social distancing brought to the safeguarding enquiry process, including being unable to undertake essential face-to-face visits. The practicalities in progressing safeguarding enquiries became more difficult. which made Making Safeguarding Personal more challenging. The COVID-19 pandemic and lockdowns created complexity and barriers in how people could report as well as experience abuse and neglect.
There was considerable variation between councils’ experiences regarding safeguarding activity in the pandemic and many variables were at play including: the number of ‘anxiety referrals’ received; proactive/preventative approaches taken; local demographics; the local provider profile; how safeguarding concerns and Section 42 enquiries are recorded; partnerships dynamics to enable effective multi-agency working; localised lockdowns coming into force; the complexity of safeguarding concerns and enquiries themselves and COVID-19 related safeguarding issues emerging and manifesting across various abuse and neglect categories.
Councils and partners adapted to maintain safeguarding roles and responsibilities during the COVID-19 pandemic, regardless of the situation that they were facing. Very specific barriers arose from the COVID-19 pandemic including reduced face-to-face contact, significantly increased workloads. In response Council innovated and adapted their communication methods, developed their approached the Section 42 enquiry process; improved how they worked with other agencies; increasing the frequency of meetings using technology; created new partnerships; increased professional curiosity; worked flexibly; and proactively to create bespoke solutions to issues that emerged. Councils developed new strategies, anticipated change, were proactive and adaptive, based on local circumstances and learning from experiences in the first lockdown.
Both Insight Project reports have been used by councils, Safeguarding Adults Boards (SABs), and partners to benchmark, reflect and identify issues within their locality to support learning and change. At the launch of the second Insight Report, presenters described how they used the national work to inspire, compare and inform local safeguarding planning and activity.
Methodology and participation
As the previous Insight reports acknowledged, the national median experience of safeguarding concerns and enquiries provides a very definite pattern where safeguarding concerns went down during lockdowns nationally, especially early on in the lockdowns, and those downward trends have become less pronounced with the pandemic continuing. The qualitative data shared by the 50 councils was sometimes about reflecting patterns found in the quantitative data, but unlike the two previous insight project reports, the qualitative data in the third iteration does not seek to provide a complementary narrative to quantitative data. Instead, the qualitative data is capturing specific phenomenon and how councils are experiencing and responding to adult safeguarding within a pandemic. The quantitative data instead captures the ongoing challenges that councils face, broadening of adult safeguarding enquiries, increasing in complexity, creating new ways of working and reassessment of service provision, policies and procedures.
The qualitative data describes the individual experiences of councils, and there was significant variation across country. As acknowledged in the previous Insight reports, variation was influenced by:
- Levels of ‘anxiety referrals’
- Local emergency services’ approaches to risk
- Changes in the location of abuse (decreased levels of safeguarding concerns and enquiries in care homes and nursing homes as a percentage share in lockdown periods in 2020 and an increase in concerns and Section 42 enquiries in the individual’s own home)
- The demographics of a locality which impact on different referral rates
- Recording methods for concerns and enquiries, which are not uniform
- Variation of the reproduction rate or ‘r rate’ and subsequent locality lockdowns;
- How technology and innovation was used in local areas
- Proactive/preventative initiatives employed by a council
- Partnership dynamics in a particular locality to enable effective multi-agency working and/or
- the complexity of safeguarding concerns and enquiries themselves and COVID-19 related safeguarding issues.
Methodology: quantitative data
As with the first and second Insight reports, requests were made for local insight and data on safeguarding activity on a voluntary basis from councils in England for the period up to June 2021. This voluntary collection of safeguarding activity compares monthly levels over time, and between equivalent months in 2019, 2020 and 2021, and month by month trends. As with the previous collections, a simplified subset of the Safeguarding Adult Collection was used, with a series of questions included to elicit further insight and intelligence on local trends and changes to provide the quantitative findings. Councils were able to participate using an online data collection form distributed electronically, which included the facility to download an Excel template and re-upload it once completed, in addition to a variety of qualitative insight questions. The quantitative data from this return was collated through LG Inform and put into charts and tables for this report. The qualitative data was collated and analysed to generate the findings.
The first Insight report presented data covering the period from January 2019 to June 2020, receiving responses from 92 councils – around 61 per cent of all single tier and county councils in England. The second Insight report presented data from January 2019 to December 2020 and is based on the responses of 101 councils – around 67 per cent of applicable councils. The third Insight report presents data from 106 councils – around 69 per cent of applicable councils. These response rates varied by region (see Figure 1 below). However, these rates refer to the percentage of councils who provided data for at least one month in the entire period from January 2019 to June 2020, including those who took part in the first or second data collections but not the third. Month by month, the percentage of councils providing data has steadily declined, reflecting an expected decrease in response rates due to a number of factors, including respondent attrition and the decline in the relative importance of COVID-19 related issues to adult safeguarding following the recent removal of government restrictions. The monthly response rate is show in Figure 2 below.
The graph above shows participants in the project as a percentage of applicable councils, second and third insight reports: Bar chart showing an overall increase in participation in the safeguarding insight project between the second and third reports, rising from around 67 per cent to around 69 per cent between these reports. The chart also shows considerable variation by region: the East ADASS Region had a 100 per cent response rate as of the third report, whereas the North West ADASS Region had a response rate of around 52 per cent.
The chart above shows percentage of adult social care councils providing data for each month: Line chart showing that month by month, the percentage of councils providing data for the project fell from around 68 per cent, at the time of the first report, to around 60 per cent, at the time of the second report, to around 40 per cent, at the time of the third report.
Councils were asked to reflect and respond to the following questions:
- Have you identified any differences in safeguarding activity between the first, second and third waves of the COVID-19 pandemic?
- Have you noticed specific safeguarding issues that have arisen for particular groups?
- Have you noticed disproportionate levels of complexity of safeguarding activity?
- What would you identify as specific learning from safeguarding work during the pandemic, and how have you changed your approach to safeguarding adults?
- Is there anything else that you would like to tell us about safeguarding activity during the COVID-19 pandemic?
This, third round of the Insight Project received the highest level of participation with qualitative responses from fifty councils. They provided detailed reflections on the questions asked. Like previous contributions, councils offered very sincere and refined answers that help paint a picture of new ways of working, responding to the challenges they faced, as exciting innovations, creating more choice, systemic change and learning. Whilst the data showed the breadth of experiences across the country, in the face of a pandemic, councils showed their ability to adapt, learn, analyse and modify; they challenged themselves to change their service in direct response to the demands raised by the pandemic. Their responses are included alongside relevant sections, and in explored in Section 7.
About the report
Individual council data is treated confidentially in this project: this report does not identify any specific individual or council, instead showing the overall picture of the situation. Identifiable information about individual councils and respondents is used internally by the LGA but is only held and processed in accordance with the LGA privacy statement. Councils were asked if they could be named in the case studies, and certain other outputs from this project will be shared privately among the councils participating in the project with their consent.
Caveats
The pandemic and its impact varied across different parts of the country. The sample of councils participating in this project, whilst of significant size, is self-selected and therefore may not be fully representative. However, enough councils have participated to provide a broad picture and provided rich and valuable data of what has been happening in England regarding safeguarding activity during the COVID-19 pandemic.
In terms of the numerical data, it should be noted that data collected from April 2020 will not necessarily be validated, so there may be potential discrepancies to the validated figures submitted to NHS Digital. Further there have been some inconsistencies in the ways in which safeguarding concerns, safeguarding enquiries and other enquiries have been reported and work has been done to address this (recommended resources include: Making decisions on the duty to carry out Safeguarding Adults enquiries and Understanding what constitutes a safeguarding concern and how to support effective outcomes), which has been supported by the adult safeguarding workstream of the CHIP. Some participants in the first phase of the project commented that practice has improved between 2019 and 2020.
Structure of the report
This report is in three sections parts 1-6 summarises the quantitative data from the Insight collection; part 7 summarises the qualitative data; and part 8 includes relevant data from the NHS Digital’s Safeguarding Adults Collection. A brief executive summary of the findings is included to help readers navigate the full report.
Summary of findings
The following gives an overview of the findings of the report. These findings are provided in more detail in each of the following sections.
Part 1: Safeguarding concerns
Safeguarding concerns show a long-term upward trend, tending to decrease during periods of lockdown and other COVID-19 restrictions, followed by a sharp increase once those restrictions are lifted. The rate of safeguarding concerns, having declined markedly in March and April 2020 only to rise to new heights in July and September 2020, declined moderately into December 2020, only to rise again in the following six months, reaching the highest level on record as of June 2021. The decline in April 2020 is accounted for mainly by a decline in the rate for older people, whereas the decline in December 2020 is accounted for entirely by a decline in the rate for working-age adults. The rate for working-age adults shows a considerably greater change relative to the pre-pandemic picture than the rate for older people.
Part 2: Section 42 safeguarding enquiries
Section 42 safeguarding enquiries did not show the same upward trend shown by concerns, though they did fall and rise in line with changes in the volume of concerns. The rate of Section 42 safeguarding enquiries fell in April and December 2020, similarly to the rate of safeguarding concerns. The rate of Section 42 enquiries also exhibits a noticeable drop in April 2021, a drop which was not apparent in any of the rates of concerns. Overall, the rate Section 42 enquiries has changed little since before the pandemic, and has not seen the considerable increase by June 2021, which is apparent in the rate of safeguarding concerns.
Part 3: Understanding variation between local authorities
Variation between local authorities in the volume of safeguarding concerns and Section 42 enquiries continued to remain high, as local authorities respond to differing circumstances in their local areas. The rate of safeguarding concerns varies considerably between authorities, and it appears that overall variation has increased somewhat over time. Section 42 enquiries present a similarly wide degree of variation; for all statistics, the 2020 figures are higher than the 2021 figures, and in the case of Section 42 enquiries the figures suggests that variation between authorities has reduced over time.
Part 4: Breakdown by type of abuse
Councils commented changes in the incidence of types of abuse, specifically domestic abuse and self-neglect. They also commented on areas including homelessness and exploitation.
In general, the percentage distribution of Section 42 enquiries by types of abuse has changed relatively little across the period recorded, although some limited evidence exists that psychological abuse, domestic abuse and self-neglect have increased during periods of COVID-19 restrictions. Overall, however, Section 42 enquiries remained dominated by neglect or acts of omission and physical abuse, as has been the case throughout the period recorded.
Part 5: Breakdown by location of abuse
Perhaps unsurprisingly, the COVID-19 pandemic saw a notable relative increase in Section 42 enquiries where the risk was located in the individual’s own home. The prevalence of this location of abuse has decreased slightly since the start of 2021 but remains higher than pre-pandemic levels. Correspondingly, the pandemic saw relatively fewer Section 42 enquiries with risk located in a residential or nursing care home.
Part 6: Breakdown by outcome of enquiry
Whilst the percentage balance of outcomes of Section 42 enquiries appears not to have changed in a sustained fashion across the recorded period, enquiries with an outcome of “Risk Reduced” seem to have become slightly more prevalent during the period from May to December 2020, at the expense of outcomes of “Risk Removed”. Enquiries with outcome of “Risk Remained” persisted at relatively low but stable levels throughout the period.
Part 7: Themes from the qualitative insight data
Part 7 of the report reflects on the qualitative responses from 50 councils that constituted a ‘deep dive’ into the growing complexity of safeguarding activity, evidence of disproportionate levels of complexity attached to specific group, it is less about quantifying safeguarding in terms of numbers but more about illustrating a breadth of commentary on safeguarding activity within adult social care, which spans mental health, homelessness, substance misuse, pressure points and changes in work practices.
Councils reported on a range of factors that affected safeguarding risks and practice during the pandemic, and their responses to them. These have been described thematically below, covering: the provider market; mental health impacts; issues for people with learning disabilities; people experiencing homelessness; family carers; prevention; use of technology. Councils reported how they changed their responses, applying learning from the initial phase of the pandemic.
Part 8 NHS Digital Safeguarding Adults Collection
The picture shown by the NHS Digital Safeguarding Adults Collection concerning the age profile of involvement in safeguarding enquiries, the mental capacity of adults at risk and risk assessments and actions taken was largely one of continuity with previous financial years. Adults aged 85 and over remained the most prevalent age group to be involved in safeguarding enquiries, though the rate of individuals involved in these enquiries per 100,000 population of the same age group dropped noticeably in the financial year 2020/21 in contrast to the previous financial year. At the same time the rate of adults aged 18-64 involved in safeguarding enquiries increased, though it remained much lower than for older age groups. The mental capacity of adults at risk remained almost entirely unchanged from previous years, with where adults who did not lack mental capacity continue to make up a narrow majority of adults at risk, and adults who lacked mental capacity remaining at around 30 per cent of adults at risk. Concluded Section 42 enquiries continued to be dominated numerically by those where a risk was identified and action taken, followed by those with no risk identified.
Summary of findings
The following gives an overview of the findings of the report. These findings are provided in more detail in each of the following sections.
Part 1: Safeguarding concerns
Safeguarding concerns show a long-term upward trend, tending to decrease during periods of lockdown and other COVID-19 restrictions, followed by a sharp increase once those restrictions are lifted. The rate of safeguarding concerns, having declined markedly in March and April 2020 only to rise to new heights in July and September 2020, declined moderately into December 2020, only to rise again in the following six months, reaching the highest level on record as of June 2021. The decline in April 2020 is accounted for mainly by a decline in the rate for older people, whereas the decline in December 2020 is accounted for entirely by a decline in the rate for working-age adults. The rate for working-age adults shows a considerably greater change relative to the pre-pandemic picture than the rate for older people.
Part 2: Section 42 safeguarding enquiries
Section 42 safeguarding enquiries did not show the same upward trend shown by concerns, though they did fall and rise in line with changes in the volume of concerns. The rate of Section 42 safeguarding enquiries fell in April and December 2020, similarly to the rate of safeguarding concerns. The rate of Section 42 enquiries also exhibits a noticeable drop in April 2021, a drop which was not apparent in any of the rates of concerns. Overall, the rate Section 42 enquiries has changed little since before the pandemic, and has not seen the considerable increase by June 2021, which is apparent in the rate of safeguarding concerns.
Part 3: Understanding variation between local authorities
Variation between local authorities in the volume of safeguarding concerns and Section 42 enquiries continued to remain high, as local authorities respond to differing circumstances in their local areas. The rate of safeguarding concerns varies considerably between authorities, and it appears that overall variation has increased somewhat over time. Section 42 enquiries present a similarly wide degree of variation; for all statistics, the 2020 figures are higher than the 2021 figures, and in the case of Section 42 enquiries the figures suggests that variation between authorities has reduced over time.
Part 4: Breakdown by type of abuse
Councils commented changes in the incidence of types of abuse, specifically domestic abuse and self-neglect. They also commented on areas including homelessness and exploitation.
In general, the percentage distribution of Section 42 enquiries by types of abuse has changed relatively little across the period recorded, although some limited evidence exists that psychological abuse, domestic abuse and self-neglect have increased during periods of COVID-19 restrictions. Overall, however, Section 42 enquiries remained dominated by neglect or acts of omission and physical abuse, as has been the case throughout the period recorded.
Part 5: Breakdown by location of abuse
Perhaps unsurprisingly, the COVID-19 pandemic saw a notable relative increase in Section 42 enquiries where the risk was located in the individual’s own home. The prevalence of this location of abuse has decreased slightly since the start of 2021 but remains higher than pre-pandemic levels. Correspondingly, the pandemic saw relatively fewer Section 42 enquiries with risk located in a residential or nursing care home.
Part 6: Breakdown by outcome of enquiry
Whilst the percentage balance of outcomes of Section 42 enquiries appears not to have changed in a sustained fashion across the recorded period, enquiries with an outcome of “Risk Reduced” seem to have become slightly more prevalent during the period from May to December 2020, at the expense of outcomes of “Risk Removed”. Enquiries with outcome of “Risk Remained” persisted at relatively low but stable levels throughout the period.
Part 7: Themes from the qualitative insight data
Part 7 of the report reflects on the qualitative responses from 50 councils that constituted a ‘deep dive’ into the growing complexity of safeguarding activity, evidence of disproportionate levels of complexity attached to specific group, it is less about quantifying safeguarding in terms of numbers but more about illustrating a breadth of commentary on safeguarding activity within adult social care, which spans mental health, homelessness, substance misuse, pressure points and changes in work practices.
Councils reported on a range of factors that affected safeguarding risks and practice during the pandemic, and their responses to them. These have been described thematically below, covering: the provider market; mental health impacts; issues for people with learning disabilities; people experiencing homelessness; family carers; prevention; use of technology. Councils reported how they changed their responses, applying learning from the initial phase of the pandemic.
Part 8 NHS Digital Safeguarding Adults Collection
The picture shown by the NHS Digital Safeguarding Adults Collection concerning the age profile of involvement in safeguarding enquiries, the mental capacity of adults at risk and risk assessments and actions taken was largely one of continuity with previous financial years. Adults aged 85 and over remained the most prevalent age group to be involved in safeguarding enquiries, though the rate of individuals involved in these enquiries per 100,000 population of the same age group dropped noticeably in the financial year 2020/21 in contrast to the previous financial year. At the same time the rate of adults aged 18-64 involved in safeguarding enquiries increased, though it remained much lower than for older age groups. The mental capacity of adults at risk remained almost entirely unchanged from previous years, with where adults who did not lack mental capacity continue to make up a narrow majority of adults at risk, and adults who lacked mental capacity remaining at around 30 per cent of adults at risk. Concluded Section 42 enquiries continued to be dominated numerically by those where a risk was identified and action taken, followed by those with no risk identified.
Part 1 Safeguarding concerns
The chart above shows the monthly safeguarding concerns per 100,000 adults, aged 18+, median for England: Line chart showing that the rate of safeguarding concerns per 100,000 adults fluctuated without apparent patterns between around 58 in February 2019 and around 79 in July 2019. Following the start of the COVID-19 pandemic, this rate fell to around 56 in April 2020, but quickly rose to around 70 in May 2020 and peaked at around 84 in July 2020. The rate slightly decreased to around 72 in December 2020, though this was higher than the rate of around 61 in December 2019. Since the start of 2021, the rate of concerns has again risen markedly, rising to the highest value on record, around 97, by June 2021.
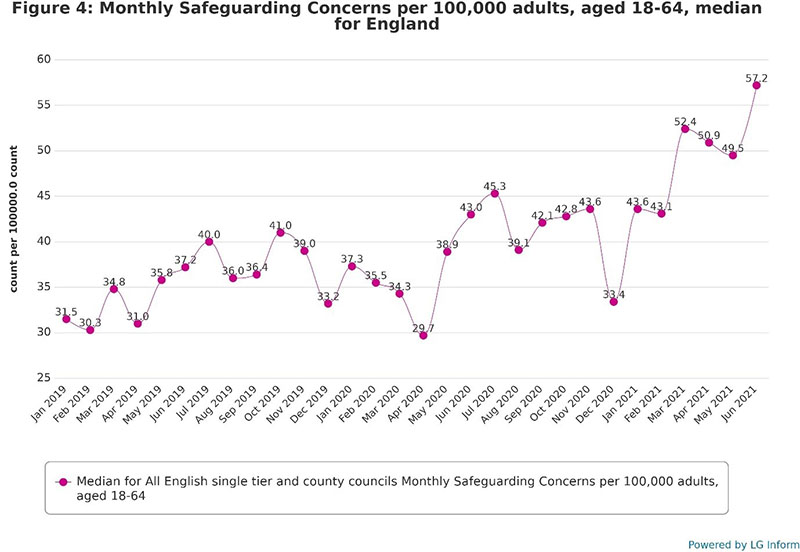
As Figure four shows, the rate of safeguarding concerns specific to working-age adults follows a roughly similar pattern to the overall rate of concerns, with temporary decreases in April and December 2020 followed by sustained increases. In general, fluctuation in the rate of concerns among working-age adults appears to have been less steep prior to the pandemic than the overall picture, with 2020 and 2021 introducing both higher levels overall and a greater degree of fluctuation. The most notable difference between the 18 to 64 rate and the overall rate since the start of the pandemic is that the drop in December 2020 is considerably more accentuated among working-age adults. Otherwise, the general trend appears to strongly resemble the overall picture.
The chart above shows monthly safeguarding concerns per 100,000 adults, aged 18-64, median for England: Line chart showing that the rate of concerns among working-age adults varied between around 30 in February 2019 to around 41 in October 2019, with noticeably less monthly fluctuation than the overall rate. The rate fell to around 30 in April 2020, though this was not significantly lower than the rate of around 31 in April 2019. It then increased sharply to around 45 in July 2020. December 2020 saw a steeper drop in the rate of concerns among working-age adults than the overall rate, dropping from around 44 in November 2020 to around 33 in December 2020. As with the overall picture, however, it then increased sharply into 2021, rising to a high of around 57 by June 2021.
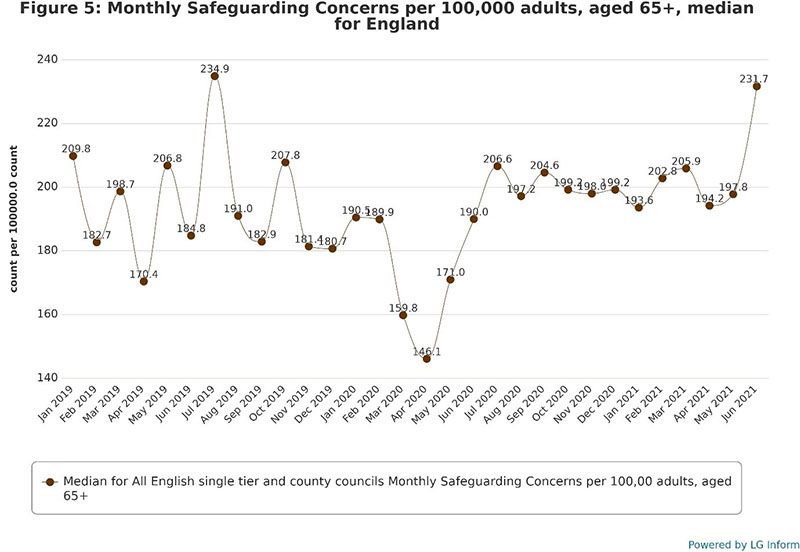
According to Figure five, the rate of safeguarding concerns among older people fluctuated far more markedly prior to the pandemic than the overall rate, in contrast to the relatively stable pre-pandemic rates among working adults. The drop in the rate of concerns in April 2020 is noticeably more pronounced than with the overall rate, although the December 2020 drop in rates is completely non-existent for the rate among older people. Instead, the rate of concerns remained almost level between July 2020 and May 2021, before increasing sharply in June 2021, although the highest rate on record remains the figure for July 2019, suggesting that the extent of long-term change in this rate is smaller than among working-age adults.
The chart above shows monthly safeguarding concerns per 100,000 adults, aged 65+, median for England: Line chart showing that the rate of safeguarding concerns among older people varied from around 170 in April 2019 to around 235 in July 2019, with steep fluctuation in this rate month by month.
Part 2: Section 42 safeguarding enquiries
The rate of Section 42 safeguarding enquiries fell in April and December 2020, similarly to the rate of safeguarding concerns. The rate of Section 42 enquiries also exhibits a noticeable drop in April 2021, a drop which is not apparent in any of the rates of concerns. Overall, the rate Section 42 enquiries has changed little since before the pandemic, and has not seen the considerable increase by June 2021 which is apparent in the rate of safeguarding concerns.
As Figure 6 shows, the overall rate of Section 42 safeguarding enquiries has always fluctuated considerably and continues to do so from the advent of the COVID-19 pandemic. The highest value in the recorded period remains that of October 201, and although the lowest value is that for April 2020, it is nearly matched by a similar low in February 2019. The pandemic, however, has seen some more systematic patterns and trends than in previous months, such as the sustained decrease in the rate of Section 42 enquiries into April 2020, and the subsequent increase up to July 2020. Since then, some degree of rapid fluctuation appears to have returned, and the June 2021 rate of enquiries has not yet risen to meet the increase in safeguarding concerns in the same month.
The chart above shows Monthly Section 42 Safeguarding Enquiries per 100,000 adults, aged 18+, median for England: Line chart showing that the rate of Section 42 safeguarding enquiries has fluctuated between around 19 in February 2019 and around 26 in October 2019. This rate fell from around 25 in January 2020 to around 19 in April 2020, before resurging to around 25 in July 2020. Since then it has continued to fluctuate considerably, falling to around 19 again in December 2020, returning to around 25 in March 2021, and falling once again to around 19 in April 2021. The rate rose slightly again to around 22 in May and around 21 in June.
As Figure 7 shows, the pre-pandemic fluctuation in the rate of Section 42 enquiries among working-age adults was considerably less pronounced than that of the overall rate. The working-age adult rate fell from a reasonable peak in January 2020 to the lowest figure in the recorded period in April 2020. This rose markedly to form the highest figure in the recorded period in June 2020, before continuing to fluctuate after that. As with the overall rate, the working-age adult rate exhibited two further notable drops in December 2020 and April 2021. One key difference from the overall rate of Section 42 enquiries is that the rate among working-age adults has risen markedly from April to June 2021, although it has yet to exceed the July 2020 peak.
The chart above shows Monthly Section 42 Safeguarding Enquiries per 100,000 adults, aged 18-64, median for England: Line chart showing that the rate of Section 42 enquiries specific to working-age adults fluctuated gently between around 10 in February 2019 to around 13 in October 2019. This rate fell consistently to around 9 from January to April 2020, before increasing steeply and steadily to around 14 in July 2020. The rate fell once again to around 10 in December 2020, returned to a peak of around 14 in March 2021, fell again to around 11 in April 2021, and has since increased once again to around 13 as of June 2021.
As Figure 8 shows, the rate of Section 42 enquiries among older people accounts for most of the pre-pandemic fluctuation in the overall rate of Section 42 enquiries. The high for the recorded period is at July 2019, although several months since then have nearly matched this figure. The rate of Section 42 enquiries among older people fell dramatically between February and April 2020, in a considerably steeper drop than that experienced among working-age adults. This rate then resurged to match and exceed earlier levels, peaking in June 2020 before once again beginning a steady decline up to a further trough in December 2020. From there the rate of enquiries rose once again to a further peak in March 2021 before experiencing a final, less pronounced drop in April and May 2021. The June 2021 figure shows another increase, though this is less pronounced than among working-age adults.
The chart above shows Monthly Section 42 Safeguarding Enquiries per 100,000 adults, aged 65+, median for England: Line chart showing that the rate of Section 42 enquiries specific to older people varied from around 57 in February 2019 to around 76 in July 2019. This rate fell sharply from around 74 in February 2020 to around 52 in April 2020, before climbing back to around 74 in June 2020. A further trough in December 2020 saw the rate fall again to around 56, then resurge once again to around 72 in March 2021. Once further drop reduced the rate to around 62 in May 2021, before increasing once more to 68 in June 2021.
Part 4: Breakdown by type of abuse
The above chart type of abuse, total for English councils: Stacked bar chart showing that across the period covered, neglect or acts of omission has accounted for around 31 per cent of Section 42 enquiries, with physical abuse accounting for around 20 per cent, psychological abuse accounting for around 14 per cent, and financial or material abuse accounting for around another 14 per cent.
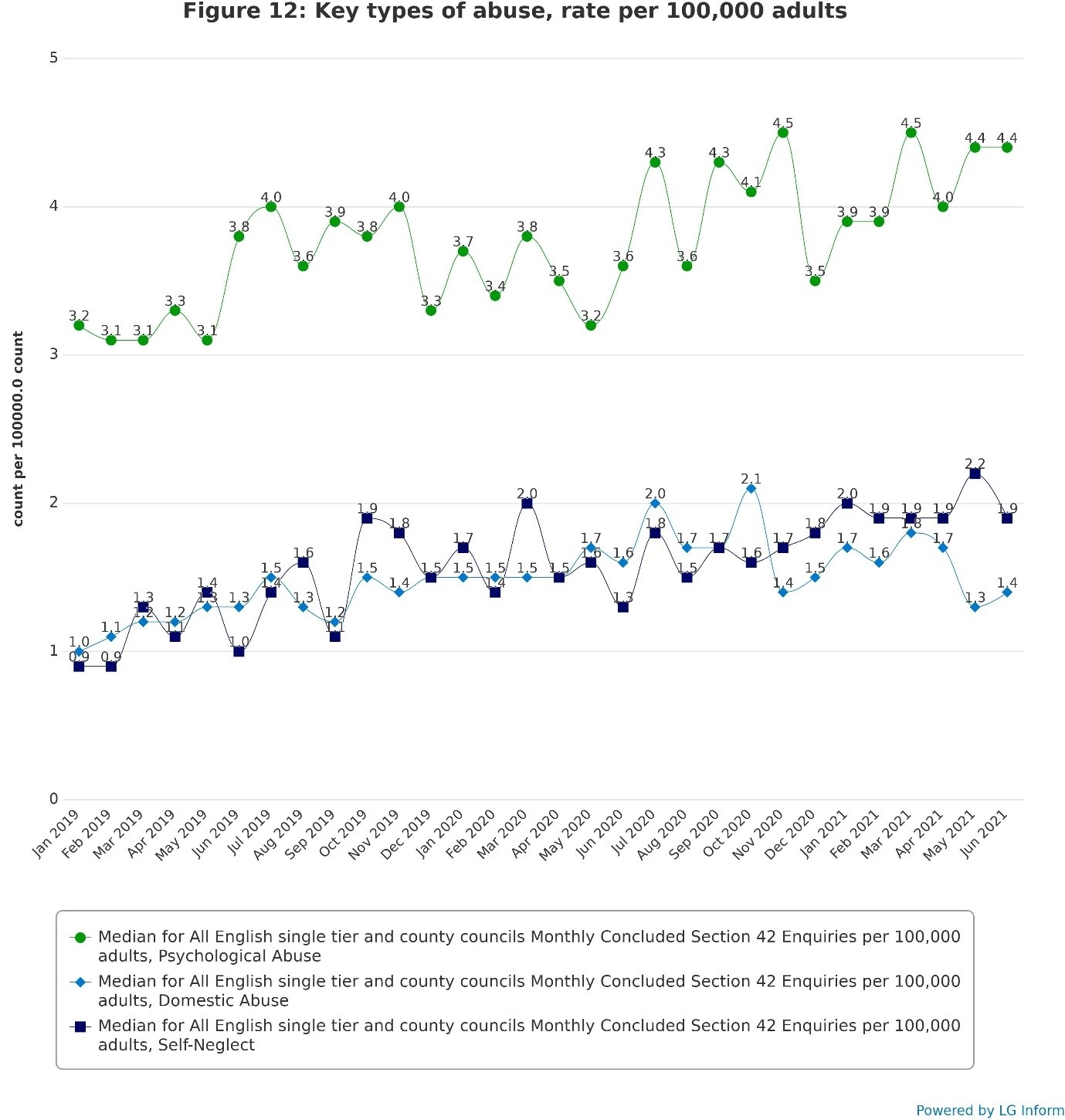
The above chart shows key types of abuse, rate per 100,000 adults: Multiple line chart showing the rates of Section 42 enquiries concerning three key types of abuse which appear to have risen slightly during the pandemic: psychological abuse, domestic abuse and self-neglect. The chart shows that Section 42 enquiries concerning psychological abuse fluctuated from 3.1 in April 2019 to 4.5 in March 2021, whilst enquiries concerning domestic abuse fluctuated from 1.0 in January 2019 to 2.1 in October 2020 and enquiries concerning self-neglect fluctuated from 0.9 in February 2019 to 2.2 in May 2021. Please note that these are rates per 100,000 population rather than percentage shares as in the previous chart and are thus influenced by the overall frequency of Section 42 enquiries as well as the prevalence of the selected abuse types within those enquiries.
Part 5: Breakdown by location of abuse
Perhaps unsurprisingly, the COVID-19 pandemic saw a notable relative increase in Section 42 enquiries where the risk was located in the individual’s own home. The prevalence of this location of abuse has decreased slightly since the start of 2021 but remains higher than pre-pandemic levels. Correspondingly, the pandemic saw relatively fewer Section 42 enquiries with risk located in a residential or nursing care home.
Figure 13 shows that the individual’s own home was already the most prevalent location of risk among Section 42 enquiries prior to the pandemic. From April 2020 the percentage of enquiries with this risk location increased markedly, with enquiries with risk located in residential and nursing care homes, the second and third most common risk locations, decreasing in relative prevalence correspondingly. There were no significant or notable changes among the other risk locations, each of which account for a relatively small proportion of Section 42 enquiries.
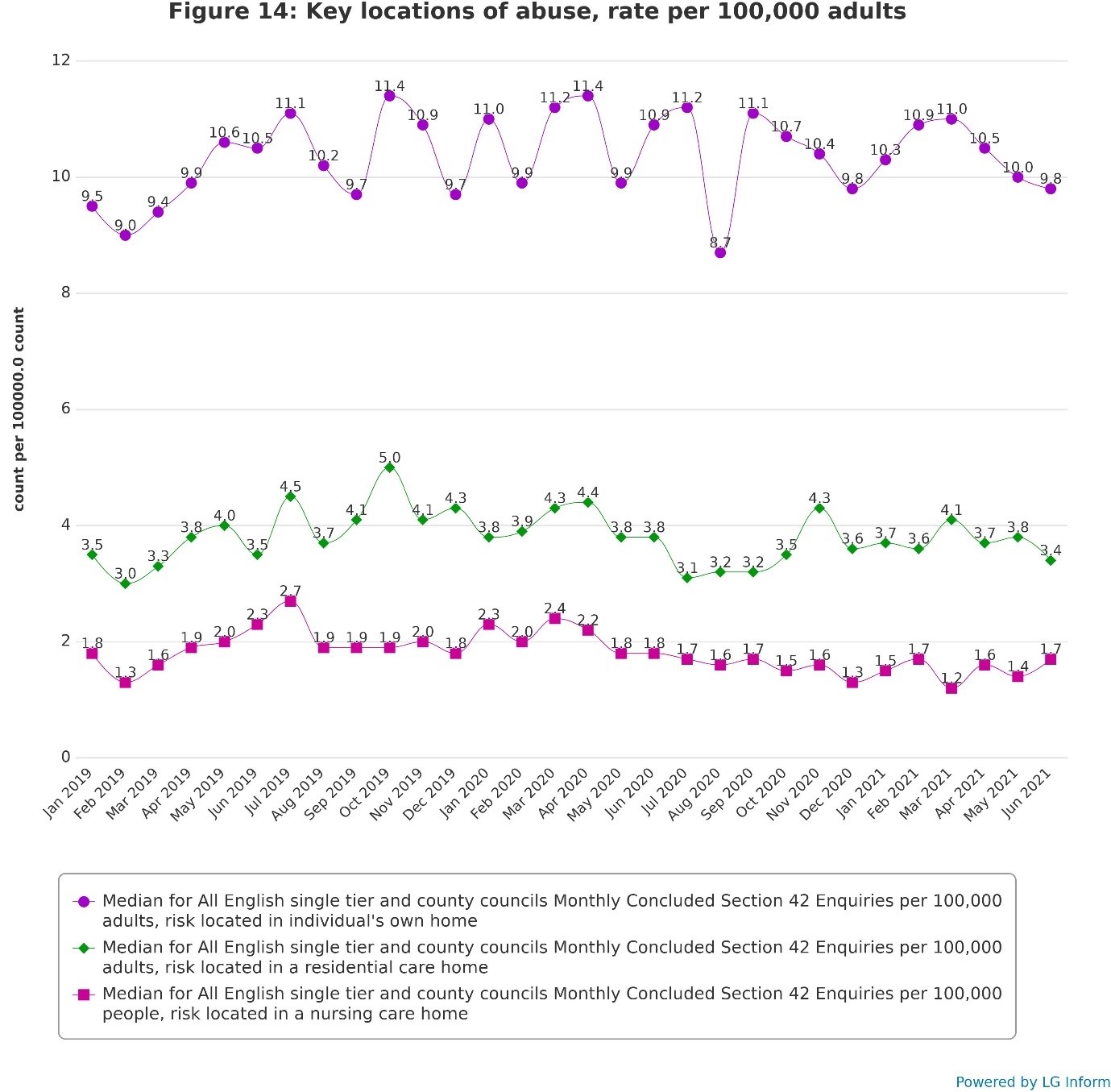
Figure 14 shows the three most prevalent locations of risk as rates of Section 42 enquiries per 100,000 adults, providing another perspective on the change in these locations of risk over time. As with Figure 12, these figures increase and decrease in line with the frequency of Section 42 enquiries as well as in line with the location of risk in question.
The chart above shows location of abuse, total for English councils: Stacked bar chart showing the relative prevalence of a range of locations where the risk is located in Section 42 enquiries. It shows that the individual’s own home, the most prevalent risk location throughout the recorded period, accounted for between 43 and 46 per cent of Section 42 enquiries from January 2019 to March 2020. From April 2020 to June 2021, this rose in a sustained fashion to between 46 and 50 per cent of enquiries. The second most prevalent location of risk, residential care homes, accounted for between 23 and 25 per cent of enquiries prior to April 2020, and for between 21 and 23 per cent of enquiries from April 2020 onwards. The third most prevalent risk location, nursing care homes, accounted for between 10 and 12 per cent of enquiries prior to the pandemic and for between eight and 10 per cent in the intervening months. The other locations of risk each accounted for less than eight per cent of enquiries, and did not change noticeably throughout the recorded period.
The chart above shows key locations of abuse, rate per 100,000 adults: Multiple line chart showing the rates of Section 42 enquiries concerning three key locations of risk: the individual’s own home, residential care homes and nursing care homes. Enquiries with risk located in the individual’s own home fluctuated from 9.0 per 100,000 adults in February 2019 to 11.4 in April 2020. It shows a notable though temporary drop to 8.7 in August 2020, likely because this is a rate per unit of population and is thus influenced by the overall frequency of Section 42 enquiries in a given month.
Enquiries with risk located in a residential care home fluctuated from 3.0 in February 2019 to 5.0 in October 2019, and has since declined to a roughly constant rate of around 3.8 since then. Enquiries with risk located in a nursing care home fluctuated from 1.3 in February 2019 to 2.7 in July 2019, and has since gradually declined, particularly from April 2020 onwards, reaching a low of 1.2 in March 2021.
Part 6: Breakdown by outcome of enquiry
Whilst the percentage balance of outcomes of Section 42 enquiries appears not to have changed in a sustained fashion across the recorded period, enquiries with an outcome of “Risk Reduced” seem to have become slightly more prevalent during the period from May to December 2020, at the expense of outcomes of “Risk Removed”. Enquiries with outcome of “Risk Remained” persisted at relatively low but stable levels throughout the period.
Figure 15 shows the percentage of Section 42 enquiries by month according to the outcome of enquiries. As it demonstrates, the most prevalent outcome throughout the recorded period is “Risk Reduced”, followed by “Risk Removed”, with “Risk Remained” as the least common outcome. There is a slight but noticeable increase in the percentage of enquiries with “Risk Reduced” between May and December 2020, mostly at the expense of “Risk Removed” outcomes but with some slight corresponding reduction in outcomes with “Risk Remained” in certain months. Since January 2021 “Risk Removed” outcomes have increased again to return roughly to their pre-pandemic levels. Outcomes with “Risk Remained” have also increased to return to their previous levels.
Figure 16 shows the three outcomes as rates of enquiries per 100,000 adults. This demonstrates that the January 2021 drop in percentage prevalence of enquiries with outcome of “Risk Remained” was matched by a drop in the actual rate of these enquiries per unit of population. The other two enquiry outcomes did not see a corresponding drop in rates of enquiries at this time, helping to demonstrate the circumstances behind the drop in prevalence of the former.
The chart above shows the outcome of enquiry, total for English councils: Stacked bar chart showing that the most prevalent outcome of Section 42 enquiries throughout the recorded period is “Risk Reduced”, which has varied between 62 per cent and 67 per cent of enquiries in this time. The second most prevalent outcome is “Risk Removed”, varying between 25 per cent and 27 per cent, and the least prevalent outcome is “Risk Remained”, varying between eight and 10 per cent. From May 2020 onwards, outcomes with “Risk Reduced” gradually increased from around 62 per cent to around 66 per cent, resulting in slight decreases in the other two enquiry outcomes.
Part 7 Themes from the qualitative responses
Qualitative data was able to capture the strategies adopted by the 50 councils who responded to the call out for more information. This helped to understand how they responded during the pandemic, what patterns they had noticed, who was being impacted and how, how they changed their responses, policies, procedures and transformed ways of working regarding safeguarding adults. Evidence shared by councils was able to shine a light on:
- preventative work developed or having to be paused during the pandemic;
- increased layers of complexity in safeguarding situations that were brought into sharp focus in the pandemic;
- closer working with partners to identify areas of improvement or concerns;
- a range of vulnerabilities being exacerbated during the pandemic;
- the impact of issues reported to safeguarding teams much later and manifesting in more acute situations and/or
- trying to find good outcomes for a person and/or with their families during the pandemic.
The preventative, pro-active and responsive approaches captured in this report are essential to understanding the broader landscape of adult safeguarding in addition to the picture that the quantitative data in this report provides and the Safeguarding Adults Collection (SAC) returns.
Complexity
The 32 per cent (16/50) of councils sending in qualitative data, specifically mentioned increasing complexity of safeguarding concerns and enquiries during the pandemic, with reports of multiple abuse and neglect categories alongside mental health problems, social isolation, health inequalities, deprivation and poverty, homelessness, substance misuse and/or exploitation. Councils also reported an increase in the intensity of safeguarding concerns, This picture is very much confirmed by the quantitative data, which showed that, between December 2020 and June 2021, 72 per cent of councils saw an increase in levels of concerns. Councils drew an interconnectedness and amalgamation of issues for the people concerned. Both concerns and Section 42 enquiries were reported to have been presented at a more acute stage. Common themes concerned the challenges in the provider market; mental health impacts of lockdown and social isolation; issues for people with learning disabilities and people experiencing homelessness; increasing pressures on family carers; challenges regarding prevention; changing use of technology. Councils reported how they changed their responses, applying learning from the initial phase of the pandemic.
Due to lockdown regulations; many safeguarding concerns have been reported to adult social care services later than prior to the pandemic. This has been the case particularly for types of abuse, such as domestic abuse, where lockdowns have increased the isolation of those experiencing abuse. Delays in reporting safeguarding concerns or related issues have altered how have been dealt with since the pandemic. Rather than being case managed, delayed referrals have presented to adult social care at a more acute stage with severe consequences, making preventative measures more difficult to implement or requiring crisis management.
Domestic abuse
When the first lockdown began in March 2020, levels of safeguarding concerns regarding domestic abuse reported to councils were relatively low. Councils had anticipated that, as the lockdown eased, there would be a rise in domestic abuse safeguarding concerns.
There was a sharp rise of domestic abuse referrals, with 42 per cent of councils reporting increased levels of domestic abuse either, throughout the pandemic or reported as lockdown measures were relaxed. Numbers of domestic abuse safeguarding concerns varied from council to council, some reported rises of over 50 per cent, whilst a minority had seen little to no increases in referrals. This pattern was reflected in the domestic abuse related offences recorded by the police, which increased each month from April to June 2020, with the largest month-on-month increase (9 per cent) between April and May 2020. The increase coincided with the easing of lockdown measures from 13 May 2020, when it became safer for victims to contact the police (ONS, Nov 2020). However, reported domestic abuse safeguarding referrals and Section 42 enquiries only showed modest increases nationally over the duration of the pandemic. An increase was also noted in the 60+ age group for longstanding domestic abuse concerns over the 3 waves of the pandemic.
As well as an increase in volume of safeguarding concerns, there was increased complexity reported, as domestic abuse was often coupled with other safeguarding abuse types (such as psychological, financial and physical abuse, and coercive control). Issues including mental health problems substance misuse or homelessness were also mentioned alongside the domestic abuse. Furthermore, as reporting was delayed, preventative measures were not able to be deployed at an earlier stage. Offending family members working from home further increased the vulnerability of those experiencing, or at risk of experiencing, domestic abuse. Domestic abuse during the pandemic has been exacerbated by social isolation and loss of support networks. The nature of abuse being presented was at a more severe stage, resulting in the safeguarding process taking longer to resolve and increased levels of risk and harm for victims. There were reports of an increase in domestic homicide reviews. The pandemic and lockdowns further hindered availability and ability of professionals to respond as they might have done in pre-lockdown/pandemic times.
Councils described an increase in the reporting of carer breakdown in domestic abuse situations, which put a strain on the family dynamic and the safety of the adult with care and support needs. One council identified how videoconferencing had enabled some domestic abuse victims to be more likely to attend safeguarding meetings, as they were able to participate in the meeting but had the option to leave their cameras off. Another council articulated how helpful the previous ‘Insight report highlighted the concerns of safeguarding professionals around the rising numbers of domestic abuse cases’ to know that they were not an outlier and put measures and provisions in place accordingly.
Increased isolation, loss of support networks and working from home are all factors that have increased the vulnerability of those experiencing, or at risk of experiencing, domestic abuse; this concern has received high media attention during lockdown. Adult Social Care (ASC) responded to the challenge by reviewing systems, processes and staff awareness in relation to the response from those people experiencing domestic abuse are identified as having care and support needs, as well as developing greater practitioner awareness of domestic abuse support organisations to enable effective signposting.
ACS has developed the learning and development offer to practitioners with training available to all staff on domestic abuse awareness, Domestic Abuse Bill and specialist training to promote the provision of effective support with those who may be difficult to engage with through greater understanding of the Trauma Informed Approach.
Self-neglect
Councils reported an increased number of self-neglect safeguarding concerns and enquiries, over the course of the pandemic. Nationally, based on the quantitative data shared there was a small increase in reporting of safeguarding concerns and Section 42 enquiries. However, in the qualitative data 60 per cent of councils specifically mentioned self-neglect as a significant issue, with 54 per cent saying that there was an increase in the level of self-neglect reported (noting also increased levels of complexity). Those referrals received during the pandemic tended to come from friends, neighbours, volunteers, which included people who were previously not known to adult social care. As lockdown restrictions were relaxed, self-neglect referrals increased, from a between a slight to a sharp increase and tended to be referred in by professionals, when they were able to visit.
A significant number of councils, regardless of the number of self-neglect referrals they received, experienced greater complexity, often alongside multiple abuse types and associated issues, which manifested in very specific ways in for example older and younger age groups. Also, some self-neglect cases were being shifted from care management casework to safeguarding casework. Complicating factors accompanying self-neglect were: mental health issues, isolation from lockdown restrictions, substance misuse, domestic abuse, obesity and homelessness. There were also challenges with engaging with services and there were attempts to counter this by creating multi-agency safeguarding cells/forums or subgroups, etc. Vulnerabilities appeared to be exacerbated during the COVID-19 pandemic in a similar way to health inequalities.
Financial abuse, exploitation and organisational abuse
Several councils mentioned an increase of financial abuse referrals regarding family members, fraudulent applications for credit cards, stealing of pensions, friends and neighbours being paid disproportionately for support, financial abuse from paid carers and financial scams. This continued into the third wave of the pandemic, including with issues of financial abuse by paid carers.
Financial abuse of people with learning disabilities from their friends and families was reported as well as being targeted for COVID-based scams, which could come in the form of telephone calls, texts, phishing (scam emails), social media, fake websites and on the doorstep scams.
Other councils reported an increase in levels and complexity of gang violence and drug related abuse such as cuckooing and exploitation.
Four of the 50 councils participating reported increases in organisational abuse that were linked to closed environments, other councils make very little mention of it. The quantitative data shows a large variation between councils but overall does not show a decline in organisational abuse. One council described an increase in organisational abuse referrals, which they partly attributed to considerable pressures and demands placed on the care sector.
Age specific issues
Accounts shared by councils, showed how abuse and neglect in pandemic conditions could in specific very differently and age-related issues have emerged.
Young adults
Five councils (10 per cent) reflected on challenges in responding to a growing level of referrals and issues regarding young adults. Two councils specifically identified the needs of young people in transition into adulthood and difficulties with the application of care and support needs criteria under the Care Act, particularly under pandemic conditions, resulting in not being able to access services, where previously they had been supported by children’s services. One council highlighted the impact on specifically on young adults with autism and/or learning disabilities, which reflected broader issues for adults with learning disabilities and autism.
Concerns about the mental health of young adults was an issue that featured alongside safeguarding issues. One council identified a number of deaths of young adults on railway tracks, all of whom were known to mental health services. A higher number of situations involving young adults engaged in risky behaviour were reported, which was exacerbated by lack of community resources and support, due to the lockdowns. One council reported that young people with mental health or other issues were vulnerable to being involved in gang related activity and receiving associated injuries. Ongoing concern regarding gang related activity for young adults increased as lockdown restrictions were eased. The councils identified increases of domestic abuse, neglect and acts of omission amongst younger adults. One council found that there had been a slight increase in the complexity of self-neglect concerns amongst young adults over 20 year of age.
Older people
There is evidence of the disproportionate impact of the COVID-19 pandemic on older people. Public Health England in their review of disparities of risks and outcomes (COVID-19: review of disparities in risks and outcomes - GOV.UK (www.gov.uk) identified that the chances of dying from COVID-19 are 70 times higher for those aged over 80 and 50 times higher among those aged 70-79, compared to people under 40 years old. Additionally, older people are also more likely than younger people to have underlying health problems. An Age UK study (The impact of COVID-19 to date on older people’s mental and physical health) drew attention to social isolation that particularly impacts on older people’s mental and physical health, and the feelings of lack of purpose or structure that lead to cognitive decline, particularly those diagnosed with dementia. It was significant that the majority of people living in care homes are over the age of 80 and between 16 March 2020 to 30 April 2021, 41,675 care home residents died of COVID-19, (Care home resident deaths registered in England and Wales, provisional, ONS, May 2021), these deaths represented a quarter of all deaths among care home residents.
The Local Government Association’s publication, Age and gender – The Impact of COVID-19, drew attention to the particular experience of older people in care homes, and the sharp increase in deaths. Enforcement of strict rules restricting visits from family and friends to protect against the disease often extended older people’s isolation and loneliness. In their responses, councils identified how care homes were concerned when there were “poor” or “failed” hospital discharges in order to free up beds (including discharges with pressure care concerns). Safeguarding risks were identified regarding carrying out nursing tasks after hospital discharges, which care homes felt unequipped to deal with, particularly where there was poor communication about the COVID-19 status of the person.
Reporting on safeguarding activity appears to have been affected by the lockdowns; during the lockdown periods, reduced visiting of care homes by family, friends, practitioners and professionals resulted in decreased numbers of concerns reported. There were different approaches to deal with this, some councils were dependent on providers to be the “eyes and ears” to identify safeguarding issues and they noted that these were not always recognised or reported particularly when the source of abuse was care home staff. Whilst other councils created alternative processes such as proactive contacts, creating provider networks to share concerns, virtual contacts and/or oversight groups to identify safeguarding issues as they arise or reoccurring issues.
In contrast to care homes, there were increased reporting of safeguarding concerns in other locations, such as community spaces and in own home environments. During the pandemic, some councils documented increased reporting of longstanding domestic abuse in the over 60s age group. One council noted increases in the number of deaths of older people that met the requirement for domestic homicide reviews. Another council reported that the largest increase of safeguarding concerns was regarding older people. A further council said there was a slight increase in the complexity of self-neglect concerns in the over 50s age group.
Whilst not exclusively impacting older people, pressure sores issues greatly affected older people. With delays in seeking help during the pandemic, three councils reported a sharp increase in referrals related to pressure ulcers (associated with neglect), most notably in care homes and hospitals, with increases in pressure ulcers around the face associated with oxygen masks. There were increased referrals regarding older people not previously known to services, particularly referred by hospitals. These also appeared due to people delaying seeking medical support, by which point skin damage had appeared.
COVID-19 – the disease, social isolation and changing guidance
During the first wave of the pandemic councils saw a number of safeguarding concerns that were COVID-19 specific. Services grappled with newly applied lockdowns, families as carers in a pandemic with less or no support. Care homes, families and agencies struggling with new and changing government guidance. Concerns were received for care home residents not going to hospital to receive treatment because of the fear of catching COVID-19, tenants of supported living schemes reported people not abiding by social isolation rules, care homes being expected to carry out nursing tasks, issues with unsafe hospital discharges back to care homes and community with lack of inaccurate or poor communication about the COVID status of the individual. This led to great pressure within residential care settings. Concerns were received about lack of Personal Protective Equipment (PPE) equipment or staff not using PPE equipment appropriately. However, subsequent waves of the pandemic have seen councils and partners adapt to the changing landscape of COVID-19, developing strategies to support the provider market, using relationships, networks and forums to share up-to-date guidance, clear up misunderstandings or confusions, identify issues as they arise, to use technology where appropriate and work in partnership with care providers and others to respond to the huge challenges created by to the pandemic. Learning how to “work within the new normal” was a key modus operandi that councils have adopted.
Provider market
Some councils described ongoing and increasing challenges in the provider market, with the third lockdown seeing their providers struggling with staffing shortages, resulting in safeguarding concerns. Throughout the pandemic, some local care providers struggled with changing government guidance, limited supply of PPE, however PPE was not mentioned as an issue in the second and third waves. Providers continued to report challenges with staff sickness. They found managing expectations of families challenging, whilst ensuring they did not breach Human Rights Act 1998 Articles 5 of the (protects rights to liberty and security) and Article 8 (protects rights to rights to a private and family life) during the pandemic. One council described this as a “whole system failure” in their locality due major challenges regarding staffing resulting in not able to respond as previously, and these factors making prevention and risk management a significant challenge.
Councils responded to the range of pressures, often providing intensive support to a number of providers including independent hospitals, domiciliary care services and care homes. Councils described how they responded to challenges through developing closer relationships with providers (and other partners – see below). One council saw a reduction of safeguarding referrals from registered care providers over the past 18 months as a result of supporting providers (residential, nursing homes, supported living, extra care housing, and domiciliary care providers). They had been proactive in their engagement with care providers, which included working with public health and infection control colleagues and the sector in turn had been receptive to this, and they want to continue this network and support into the post-COVID-19 landscape.
Whilst councils have been putting in place systems and structures to support the provider market, they have reported that they have been struggling with the impact of the pandemic on those providers with weaker leadership. Staffing issues, recruiting and retaining staff of a sufficient quality, have been cited as ongoing challenges. Skills for Care’s report, The State of the adult social care sector and workforce in England 2021, highlighted that the levels of staff sickness nearly doubled in the over the course of the pandemic (reasons included self-isolating and childcare issues). Further, they estimate and average of 105,000 vacancies are being advertised every day. Whilst vacancy rates fell during the start of the pandemic, since May 2021, vacancy rates have gradually increased as the wider economy has opened up. As of August 2021, vacancy rates were back above their pre-pandemic levels. Based on data collected since March 2021, Skills for Care found that: ‘there was a sharp drop in the number of people arriving in the UK to take up adult social are jobs (1.8 per cent of new starters in January-April 2021 compared to 5.2 per cent during the same period in 2019)’.
Mental health issues
Councils emphasised the prominence of mental health issues in many of the safeguarding concerns and enquiries. Mental health teams working with safeguarding teams reported declining mental health throughout the pandemic, linked to increased social isolation, homelessness, self-neglect, substance misuse, suicide ideation, self-harm and domestic abuse. Deterioration of mental health due to financial difficulties was reported to increase during the pandemic. Councils reported that mental health services experienced an increase in referrals across the board, which included a number of people becoming known to secondary mental health services for the first time. Safeguarding issues relating to exploitation, including gang violence and drug related abuse such as cuckooing was usually related to mental health needs and substance misuse. Some significant self-neglect cases were described as relating to mental health needs caused by increased anxiety due to COVID-19, exacerbated by lack of being able to get out, as well as lack of visits by family, friends or professionals. A feature captured by one council was the impact of mental health problems on young adults with autism and or learning disabilities and adults of working age during the pandemic. There were examples shared involving police where adults were presenting with a mental health need.
People with learning disabilities
Across the three Insight reports, councils noted non-compliance with public health measures, especially in the first lockdown by some adults with learning disabilities. Early in the pandemic, there were misunderstandings surrounding the COVID-19 lockdown guidance, which resulted in increased work for councils. Specific issues arose, such as managing disagreements between providers and family carers, especially when a parent was insistent on seeing their children against pandemic guidelines. Councils reported that this situation has improved over the period of the pandemic. However, many councils during the second wave of COVID saw a continued increase in financial abuse and scamming of people with learning disabilities, specifically from friends and family.
Over the duration of the pandemic there was increased use of videoconferencing with people with learning disabilities, which had a mixed response. For some people with a learning disability the use of virtual formats had a negative impact on them, others preferred the use of remote meetings. Some teams continued with face-to-face meetings where there were urgent visits (as required). Safeguarding teams have been thinking more creatively about ensuring that councils offer a wider range of meeting arrangements and to ensure that they are best able to communicate with a person that is most appropriate to that person and situation.
Homelessness
The government initiative, ‘Everyone in’, was intended to ensure all rough sleepers and those with shared air space in homelessness accommodation were provided with a safe space to reside in a hotel and emergency accommodation in order to reduce their risk of contracting COVID-19. Whilst the ‘Everyone in’ initiative was welcomed by councils, issues were highlighted including removing barriers for those who did not have a local connection and those who had no recourse to public funds (see Crisis’ response paper which outlines some of the barriers that councils faced).
‘Everyone in’ created an opportunity for councils to engage with people either experiencing homelessness or had insecure accommodation, which provided opportunities for safeguarding teams to support those people who previously they did not or could not engage with who had care and support needs. Many had not been assessed and/or were not known to adult social care and were able to be provided with health and social services, as well as move into accommodation. Councils reported that, as lockdown restrictions eased, visits also increased, which resulted in increased reporting of safeguarding concerns. These referrals cited substance misuse, mental health, self-neglect, exploitation and domestic abuse issues linked to safeguarding risks. Councils reported that, although accommodation was provided, people continued to experience many safeguarding abuses and neglect and required ongoing support which some councils found very challenging. Challenges included trying to find a place of safety for those experiencing domestic violence and/or ‘honour’ based violence. As localities entered the second and third waves of the pandemic (or additional lockdowns that were locality specific) additional resources were required regarding mental health support.
For some locality teams and Multi-Agency Safeguarding Hubs (MASHs), this was new safeguarding activity, and they reported that they were being asked to assess people who had “previously fallen through the gaps”. One council said how they were engaging with people who experienced homelessness more “assertively” and that this had given them an opportunity to look at the services and support that they offered. Councils were also looking at how they were applying the criteria for assessing safeguarding in the context of homelessness, others created teams to focus specifically on people experiencing homelessness, multiple disadvantage and complexity during the pandemic and as a result commissioned a new high needs service.
Friends and families and the role of family carer
Councils described the increasing pressures during the pandemic on family carers and members who were part of the essential workforce. having to go out to work, others who had lost or reduced livelihoods, or were working from home. This could lead to higher levels of deprivation, ill health, catching COVID-19, feeling isolated, having reduced or no access to services for their family member with care and support needs and no respite support. Any of these situations could cause increased stress, which could result in breakdown of relationships and inability to care for their family member.
Carer stress was often mentioned by councils, often due to lack of access to services or support, including access to day centres or short breaks. There were also incidences described where other family members were unable to provide support which they previously had been able to provide, due to lockdown issues, infection control concerns or the need to change employment patterns as lockdown affected various services and industries, which led to further increased pressure on carers. Some families and/or informal carers declined support from outside agencies due to infection concerns, even though it was available. There were reports of increased family members conflict and increased domestic abuse. There were cases where families where there were older people as carers were unable to cope with partners and family members and were unable to provide the increased care required.
For those with family members in care homes or other closed environments there was frustration at not being able to have face-to-face contact with their family member or visit. This sometimes led to safeguarding concerns due to non-compliance or family conflict (which could lead to an increase in family members raising concerns against each other in relation to precautions taken or not taken). Families expressed concerns about PPE being used inappropriately, the lack of PPE equipment for staff and the lack of testing for privately arranged carers, at various points throughout the pandemic. There was confusion expressed by families, agencies and care homes regarding changing government guidance. Ambulance services were the source of increased safeguarding referrals where packages of care or increased packages of care were needed.
Reduced preventative work
Due to the pandemic many councils reported having been unable to undertake some of their regular preventative work within the community, including pop up safeguarding stalls and interaction with community and voluntary groups. As mentioned above, many safeguarding concerns were being referred at a later stage due to lockdown conditions and this resulted in higher levels of risk and more severe and complex situations, making it more difficult to use preventative strategies. This placed significant pressures on the specialist safeguarding teams, particularly.
Increased levels of blue light service referrals
As has been described in the two previous Insight reports, there were high level of safeguarding referrals reported from the police and ambulance services. Many of the police or ambulance services made safeguarding referrals involving people presenting with mental health problems, self-neglect, financial abuse, domestic abuse, people in crisis, sometimes where packages of care or increased packages of care were needed these referrals spanned across all age groups. There were cases were families and partners were finding it difficult to care for their family member and were unable to provide the increased care needed. This pattern has continued throughout the pandemic period.
Technology: virtual and face to face meetings
Almost all councils have mentioned that the increased use of technology has enabled compliance with stay-at-home orders during lockdowns. During the pandemic, safeguarding teams were able to undertake and support virtual assessments (including safeguarding enquiries), strategy meetings, information sharing, training sessions, webinars, with the use of technology. One council mentioned how they used technology to support Best Interests Assessors (BIA's) through WhatsApp. Some councils said they had seen more engagement from individuals and families as they had more flexibility to attend virtual meetings. The use of technology enabled increased frequency of meetings, a wider range of professionals around the virtual table, particularly professionals such as General Practitioners who previously had been less able to attend, due to their work patterns and travel time to meetings. Councils also described how co-ordinating strategy meeting arrangements was easier. Some councils noted that it enabled a higher participation of people experiencing domestic abuse. Some neurodiverse adults were reported to have found technology enabled them to better access Adult Social Care (if they had access to broadband and the appropriate technology). Use of technology also enabled those people who had experienced abuse and/or neglect to have the option to participate in the meeting but leave their cameras off. Other councils experienced reduced number of people with care and support needs attending safeguarding meetings
Also, councils reported that practitioners have been using assistive technologies such as smart speakers (such as Alexa, Siri and Google) to set reminders and alarms for example and provide alternative ways to support people, such as use of medical dispensers to support management of medication.
Councils identified some challenges with virtual communication, particularly to make effective use of advocacy. Many councils also reported not being able to access care home settings early in the pandemic, which impacted on the effectiveness of enquiries, and particularly advocated the value of visits to care homes. Subsequently improved processes and contact using technology where appropriate addressed these issues.
Many councils acknowledged the importance and value of face-to-face contact and relationship building, described in terms of the “best way for personalised responses to safeguarding concerns”. Many expressed a prudent use of virtual communication, opting for safeguarding teams having far more face-to-face meetings instead of virtual, particularly for home and care provider visits. Learning from the first wave of the pandemic, councils report that there is a more nuanced and risk-based approach to face-to-face contact
During the first wave of the pandemic there was a decrease in the number of practitioners entering registered locations, COVID-19 restrictions eased, and practitioners accessed COVID-19 vaccinations, so did the level of visits to registered locations increase. In some instances safeguarding teams have resumed the previous ‘business as usual’ approach, especially care home visits, responding to organisational abuse concerns and/or where there are concerns about ‘closed cultures’.
Hybrid approaches have been seen as the way forward. Most councils were embracing videoconferencing, and often councils described a combination face-to-face visits and technology to best support the adults choice about their involvement in the safeguarding process. Councils have continued to deliver safeguarding duties and enquiries and standard practice has been enhanced through use of technology.
Partnerships and multi-agency working
The COVID-19 pandemic had brought a sense of urgency and necessity in the formation to new partnerships and multi-agency arrangements. The majority of councils have described stronger and regular engagement with partners. They “embraced” working in partnership, taking a multi-agency approach, which was further enabled through the use of technology allowing engagement with partners who had restricted time and ability to attend safeguarding meetings. Councils have adapted and become more flexible and responsive to changing demands, describing how existing multi-agency partnerships have been strengthened and more aligned and new partnerships have been developed. Councils and Safeguarding Adult Boards (SABs) have developed teams, partnerships and processes to create opportunities for early intervention, strengthen place-based partnerships, seek assurances, mitigate risks and/or identify emerging themes. The case studies below illustrate these themes.
NYCC redeployed team members from elsewhere in the council to form a Care Setting Support Team, which worked within existing quality and market development team. The team has operated over seven days making daily calls to all 233 care homes and extra care settings at the height of the pandemic to proactively check on the situation in care homes and to offer support as necessary. We developed a menu of interventions that the Care Setting Support Team were able to refer to when speaking with providers.
The oversight from Silver and Gold meant we were able to provide a rapid response with a focus on prevention. This has required honest conversations with providers to allow us to have an accurate picture and provide timely support. Feedback from CQC colleagues was that our approach meant their inspectors did not need to make separate calls as we had an accurate view of the whole sector. Having a whole county view of the issues faced in care settings meant we were able to share learning and target individual and whole sector support. This meant that quality and safeguarding issues could be addressed and resolved effectively and promptly.
Learning from the pandemic: respond rather than react; review, redesign and/or restructure
Councils became more responsive and anticipatory as they faced the second and third lockdowns, as the pandemic progressed. Oldham Council, a case study in the second report, implemented a proactive strategy for addressing under-reporting from care homes, reflected again on how in the second and third wave they further developed the ability to be able to interpret and analyse the safeguarding data. They noted how in the first wave, they were able to respond the data, but as the pandemic continued, they analysed the peaks and trends, and were able to be much more responsive, as they were “able to predict, plan and respond”; working with commissioning, quality and CQC colleagues to prepare. This offered assurances that the strategies that were put in place during the lockdown were efficient and maintained peoples’ wellbeing and safety.”
In autumn 2020, councils reported that they were able to construct evidence-based forecasting and projections, looking at their previous safeguarding data. Some used evidence and case studies from the first and second Insight Project reports to identify and recognise pressure points in their locality. They were able to predict and make assessments based on the demographics of their locality or respond to under-reporting from particular sectors such as residential care, which nationally saw a downward trend in reporting of concerns and consequently Section 42 enquiries.
Many councils took the opportunity to take stock, reflect, restructure, rethink and/or develop their processes, procedures and strategies to ensure the well-being of the people they supported. Others also ‘baked in’ recovery and “building back better” from the pandemic, reflecting on the lessons learned, including innovation, flexibility, better ways of working, becoming more person centred in practice, ensuring professional curiosity – all experiences that have created invaluable learning for future working, despite the challenges from the COVID-19 pandemic. Drawing on experiences from the pandemic, councils have been innovating, creating flexibility in the system to overcome challenges. The case studies below illustrate some new ways of working.
Council 3 also implemented an ‘Every COVID Visit Matters’ (ECVM) process, which allowed people to feedback directly to the local authority. During the pandemic, audits were developed that included the guiding principles of safeguarding, and adherence to Making Safeguarding Personal. Looking at the preventative approaches needed and the challenge to prevent safeguarding concerns being raised. Council 3 changed their care management aiming to reduce safeguarding activity. This involved reducing incomplete care reviews and requests for assessment (which were late) and resulted in reducing the number of safeguarding referrals. Council 3 staff also utilised non-statutory enquiries (section 42 (i)), especially with people who self-neglect, applying Section 11 of the Care Act duties. This ensured that relationships were developed and people got the best quality service, given the resources constraints, throughout a pandemic. Consequently, they were able to mitigate risks and identify areas of good practice. Additionally, they valued maintaining relationships with provider services, to ensure an open, honest and transparent dialogues. As visits to care homes were limited to health professionals, including district nurses, GPs, ambulance staff and funeral directors, and neither CQC nor the in-house Quality Assurance Team were able to access care home in lockdown conditions, professional feedback from to staff was encouraged and, as a result Council 3’s feedback both was both positive and identified areas for improvement.
Case Study London Borough of Newham November 2021
Since January 2020 all adult safeguarding referrals and police merlin notifications have been screened by the Vulnerable Adults Team who sit within Newham’s Multi Agency Safeguarding Hub. The Merlin (Metropolitan Police referral system) process has now been electronically incorporated in to the Azeus electronic case management system, in order to capture valuable data in respect of repeat notifications in particular, which in turn enables more accurate mapping and monitoring of trends and themes. There is a particular focus on trying to understand those people experiencing: rough sleeping, substance use issues, personality disorders, modern slavery and human trafficking victims and those in transition to adulthood services.
In order to provide a meaningful provision for these particular groups of people a number of suggestions were made by the Vulnerable Adults Team (VAT) Manager and changes have been made to the team which includes:
- One experienced No Recourse to Public Funds (NRPF) worker integrated into the team, with an expanded brief to focus on NRPF and Modern Slavery and Human Trafficking cases, which includes a remit to develop better local data collection with support from the Vulnerable Adults Team (VAT) Manager who is also the Single Point of Contact (SPOC) for Adult Social Care (ASC) services in Newham and the chair of the Pan London Modern Slavery Leads data collection sub group;
- A complete refresh of Newham’s High Risk Panel (NHRP) ensure wider safeguarding partner involvement across the spectrum of services with an incorporation of Blue Light Change Resistant Drinker referrals now also being heard at panel, after a successful partnership set up between ASC, Alcohol Change UK and the local substance use service, Change Grow Live (CGL);
- Modern Slavery Joint Strategy being developed with Children and Younger Person’s Services (CYPS) directorate, which includes safeguarding responses required for those aged 18 – 25 designed to offer a range of measures to address both extra familial and contextual safeguarding issues.
- During the lockdown in 2020 the VAT took on responsibility for managing some of the most complex rough sleeping cases, due to high levels of uncertainty regarding what would happen to them. The Senior Practitioner in the team works as a specialist worker with local rough sleeping services and provides ASC assessment, case management and safeguarding input to the most complex cases, which allows for better partnership working and consistency and continuity of approach.
- The use of technology has been embraced during the pandemic, with lessons learnt as regards how effective communication platforms such as Skype and Microsoft Teams can be when working in partnership with safeguarding partners when time is precious, e.g. initial responses.
Part 8: NHS Digital Safeguarding Adults
The following charts are derived from data from the NHS Digital Safeguarding Adults Collection. The latest round of data, covering the financial year 2020/21 and thus much of the pandemic thus far, was published by NHS Digital on 16 September 2021. This data is on an annual rather than a monthly basis, hence is unable to capture the same monthly granularity as the findings of the COVID-19 Safeguarding Insight Project, but includes a wider range of measures than are included in the Insight Project. A selection of these additional measures are shown below, to compliment the Insight Project’s findings.
The picture shown by the NHS Digital Safeguarding Adults Collection concerning the age profile of involvement in safeguarding enquiries, the mental capacity of adults at risk and risk assessments and actions taken was largely one of continuity with previous financial years. Adults aged 85 and over remained the most prevalent age group to be involved in safeguarding enquiries, though the rate of individuals involved in these enquiries per 100,000 population of the same age group dropped noticeably in the financial year 2020/21 in contrast to the previous financial year. At the same time the rate of adults aged 18-64 involved in safeguarding enquiries increased, though it remained much lower than for older age groups. The mental capacity of adults at risk remained almost entirely unchanged from previous years, with where adults who did not lack mental capacity continue to make up a narrow majority of adults at risk, and adults who lacked mental capacity remaining at around 30 per cent of adults at risk. Concluded Section 42 enquiries continued to be dominated numerically by those where a risk was identified and action taken, followed by those with no risk identified.
Figure 17 shows the rate of adults involved in safeguarding enquiries per 100,000 adults in the population of the same age group. It shows a moderate reduction of the rate of individuals involved in enquiries among the 75 to 84 and 85 and over age groups between 2019/20 and 2020/21, with the rate among those aged 85 and over experiencing the steepest decline. Whilst it should be noted that the decline in rates of enquiries in 2020/21 is partly the result of the overall decline in enquiries in this year compared with the previous year, the rates of individuals involved in enquiries among those aged 18 to 64 rose during this period, although they remained infrequent enough compared to the older age groups for this difference to be barely discernible by comparison.
Figure 18 shows the percentage breakdown of adults at risk for the most recent three financial years, according to whether or not they were found to have mental capacity according to the mental capacity assessment outcome. This demonstrates that for 2020/21, as with the previous two financial years, a little over half of adults at risk were found to have mental capacity, with around 30 per cent found not to have capacity, and the rest accounted for by adults at risk where the results of the mental capacity assessment outcome were not known or not recorded. The only notable difference between 2020/21 and previous financial years in this regard was a slightly lower percentage of adults at risk who were found to lack mental capacity, made up for by very slight increases in the percentages of adults who were found to have capacity and adults whose outcome with regard to capacity was not recorded.
Figure 19 shows the percentage breakdown of concluded Section 42 enquiries according to the cross-classification of whether a risk was identified and whether any actions were taken. This shows that a large majority of enquiries had a risk identified and action taken, followed by enquiries where no risk was identified and no action taken, and enquiries where no risk was identified but action was nevertheless taken. As with the previous topics, changes from previous financial years remained slight, although the percentage of enquiries with risk identified and action taken decreased very slightly, met by a very slight increase in the percentage of enquiries with no risk identified and no action taken.
The multiple line chart above shows that the rate of individuals aged 85 and over involved in safeguarding enquiries per 100,000 individuals of the same age group varied from around 2,500 in 2018/19 to around 2,600 in 2019/20, before reducing to around 2,300 in 2020/21. The rate of involvement in enquiries for individuals aged 75 to 84 ranged from around 790 in 2018/19 to around 850 in 2019/20 and around 760 in 2020/21. The rate of involvement for individuals aged 65 to 74 ranged from around 260 in 2018/19 to around 290 in 2019/20 and around 280 in 2020/21, whilst the rate of involvement for those aged 18 to 64 ranged from around 125 in 2018/19 to around 141 in 2019/20 and around 142 in 2020/21.
The image above is a stacked bar chart showing that around 52 per cent of adults at risk in 2018/19 and 2019/20 were assessed as not lacking mental capacity according to the mental capacity assessment outcome, a figure which rose slightly to around 53 per cent in 2020/21. The percentage of adults at risk which were assessed as lacking mental capacity was around 32 per cent in 2018/19 and 2019/20 and around 30 per cent in 2020/21. The percentage of adults at risk with mental capacity not known remained constant throughout the latest three available financial years, at around eight per cent, and the percentage with mental capacity not recorded rose slightly from around eight per cent in 2018/19 and 2019/20 to around nine per cent in 2020/21.
The charts above show risk assessments and actions taken: Stacked bar chart showing that around 70 per cent of concluded Section 42 enquiries had a risk identified and action taken in 2020/21, compared with 72 per cent in 2019/20 and 69 per cent in 2018/19. The percentage of enquiries with no risk identified and no action taken ranged from seven per cent in 2018/19 to six per cent in 2019/20 and eight per cent in 2020/21, whilst the percentage of enquiries with no risk identified, but action remained constant throughout the three financial years at around seven per cent. Other combinations of risk assessment and action taken remained more or less constant throughout the period, with the exception of those with risk identified and no action taken, which reduced from five per cent in 2018/19 to four per cent in 2019/20 and 2020/21.