The Trust decided to implement an electronic system to find a better way of managing complex discharges in 2013. This was developed in APEX, a low-code development platform that enables an organisation to build scalable and secure apps. This example of a local initiative forms part of our managing transfers of care resource.
Patient flow and bed management are important parts of hospital management; in order to ensure there are enough beds available for additional patients entering the hospital. Sometimes patients are medically fit and ready to leave hospital but can’t leave because arrangements have not been put in place to receive them at their next point of care, for example going to a nursing home for a temporary stay or as permanent residence.
Previously this was managed through a paper process, using faxes to communicate with social services, which led to problems with transcription errors, and there was no tracking. This created a frustrating environment with little transparency and the partner organisations struggled to work cohesively.
The plan
The Trust decided to implement an electronic system to find a better way of managing complex discharges in 2013. This was developed in APEX, a low-code development platform that enables an organisation to build scalable and secure apps.
Implementation
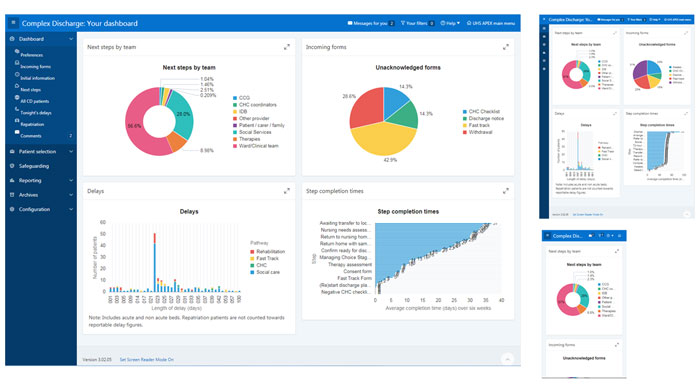
Since 2013 various iterations have been released, including a user dashboard which is designed to provide an “at a glance” status report. It is possible through the click of a button to have access to detailed information such as who is waiting for care at a patient level and the situation regarding trust wide complex discharges. This enables communication to be maximised across the system and helps to build effective relationships for what is a difficult and challenging aspect of the service management.
We can now provide so much information to support pathway transformation. We have data to show when pathways are inefficient or efficient, for example, can see how long it takes for any organisation to progress to the next step to support a patients safe discharge.
Over time we have enhanced the data quality work. In the beginning we had a regular and very long meeting to agree the situation and then sign it off. Those meetings took place every day of the week Monday to Thursday. These were usually three-hour plus meeting with paper and APEX and the updating of APEX was more of an admin exercise. Feedback from these meetings helped us to modify the system. We looked at the delay reasons and made them clearer and quicker to complete. An important part of the work with the system is the validation of the data. We can see what happened each day. We know how many forms are in the discharge bureau at any time. Now we have just one meeting of one and a half hours which is focused on troubleshooting our longest stay patients on our delayed transfers of care (DToC) List. The managers perform daily the overall validation and it takes a few mins.
We generate email alerts from the system at midnight – summarising key status – these go out system wide and support effective communication.
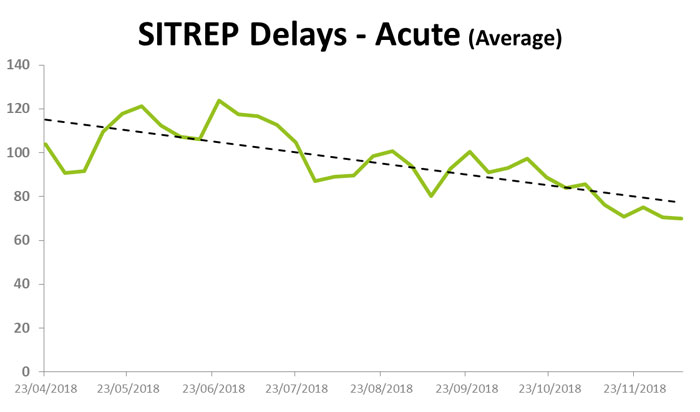
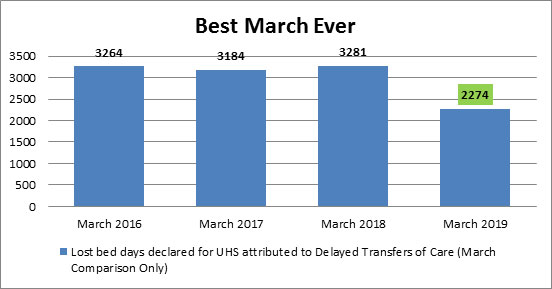
Outcomes
With manual data entry the data was very much owned by the Trust and we found that local authorities would challenge and dispute it. The electronic solution can be accessed and used by all the stakeholders including community support services and social services. With this system there is a sense of shared ownership and we undertake data validation every day, therefore the reporting is very accurate. This whole approach has built trust between the care providers.
We have now become so reliant on this system we could not operate without it.
We now can predict demand very accurately and know if patients are not discharged ,and what the overnight position on beds will be. We know when there is a big influx of patients what our discharge status is and we are able to more accurately identify patients who are not medically fit today but maybe tomorrow.
Even though we have done all this work we are still not good performers on the national leader board for delayed transfers of care. We believe this is due to challenges in our locality. We know we have genuine information and our data is very good. We know we have over 250 patients a day but it’s very unusual for us to have a patient that we don’t know about. The team work to actively liaise with the wards to get early referrals.
We are a large trust operating in a complex health and care service. The system enables co-ordination of 66 staff across seven organisations with many levels of referrals.
We use the system to work with patients families. The system enables conversations with relatives about a patient’s situation as we can easily audit the history of the actions and tell them exactly what has happened, the current status and what is planned.
Contact
Emma Rossiter, GDE Benefits Manager
[email protected]
Rachel Bailey, Integrated Discharge Bureau Operational Manager
[email protected]
Dave Waghorn, Senior Technologist
[email protected]